Rumalaya gel

Charles A. Andersen, MD, FACS
- Chief of Vascular/Endovascular/Limb Preservation Surgery Service
- Department of Surgery
- Madigan Army Medical Center
- Tacoma, Washington
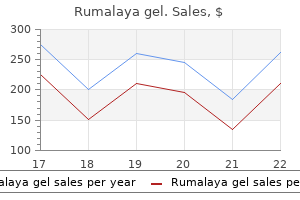
Under tissue culture conditions that starve the cell of its ability to synthesize thymidylic acid spasms 1st trimester buy rumalaya gel with american express, a chromosome break at Xq27 spasms meaning cheap rumalaya gel 30gr, the distal part of the long arm of the X chromosome muscle relaxant equipment purchase 30 gr rumalaya gel visa. Fragile X syndrome is the first recognized example of a trinucleotide repeat disorder spasms jerks order rumalaya gel overnight delivery. The explanation for this disparity in females most likely is the phenomenon known as X chromosome inactivation muscle relaxant allergy order 30gr rumalaya gel overnight delivery. Premutations and spasms during meditation buy generic rumalaya gel 30gr on line, in females, random X inactivation explain the lack of penetrance of the fragile X gene. Men with premutations, however, do not have affected sons, because they give their Y chromosome to all of their male offspring. Molecular Cytogenetic Syndromes Advances in molecular genetics have provided new insights into the genetic pathogenesis of several syndromes often associated with specific cytogenetic abnormalities. Detailed molecular analysis of the rearranged regions may help to identify the gene(s) associated a specific phenotypic presentation. Chromosomal microarray has been widely adopted as the first-tier clinical test for individuals with multiple congenital anomalies, developmental delay, intellectual disability, and autism spectrum disorders. Partial metaphase plate shows the chromosome break at Xq27 (arrow) characteristic of fragile X syndrome (solid Giemsa stain). When a female germ cell enters first prophase of meiosis, X inactivation is abolished; both X chromosomes become genetically active through fertilization and continue so until embryonic uterine implantation. Women heterozygous for either a premutation or full mutation have a 50% chance of passing it on to each child as follows: If she has a full mutation, she passes it on as a full mutation in most instances; if she has a premutation, she passes it on to her child as either a premutation or expanded into a full mutation, depending on the size of her own premutation. As the number of repeats in the premutation increases, the greater the likelihood that her premutation will expand to a full mutation in her offspring. Males affected with fragile X syndrome have cognitive impairment, ranging from severe to borderline in degree. The majority have speech delay, short attention span, hyperactivity, persistence of mouthing objects, and poor motor coordination. Many exhibit a variety of disordered behaviors, including disciplinary problems, temper tantrums, poor eye contact, perseverative speech, hand flapping, avoidance of socialization, and rocking. Physical stigmata may include long, wide, or protruding ears; long face; a prominent jaw; flattened nasal bridge; "velvety" skin; hyperextensible joints; and mitral valve prolapse. Approximately 50% of females affected with full-mutation fragile X are clinically normal. However, learning disabilities, mood disorders, schizoid personality, and significant disturbances in affect, socialization, and communication are common. The physical features often seen in males with fragile X syndrome are less common in females. Laboratory testing for fragile X mutations is done by molecular genetic techniques. These techniques can also be applied to fetal cells for the purpose of antenatal diagnosis. However, if the fetus is a female with a full mutation, it is impossible to predict with certainty whether the child will be clinically affected with fragile X syndrome after birth because of the influence of X inactivation. Rarely, an individual may seem to have a mild form of fragile X syndrome but tests are negative using these molecular genetic laboratory techniques. Disorders of Imprinting (Epigenetic Phenomena): Prader-Willi and Angelman Syndromes Etiologic Mechanisms Prader-Willi and Angelman syndromes are disorders that derive from abnormalities of imprinted genes. The concept of imprinting refers to the fact that the function of certain genes is dependent on their parental origin: maternal versus paternal. This appears particularly true of the 15q11-q13 region of chromosome 15, a region that contains several imprinted genes that, when abnormal, result in recognizable constellations of physical and behavioral problems. However, when deletion of the Angelman critical region is causative, it is the maternally derived chromosome that is deleted. The six currently identified etiologic mechanisms of Angelman syndrome include the following: 1. A large chromosome deletion of 15q11-q13 including the Angelman critical region of the maternally derived chromosome 15 (68% of cases) 2. A structural chromosome abnormality involving the Angelman critical region of 15q11-q13 (translocation, and so on) 3. Classic phenotype, with no identifiable etiologic mechanisms but a positive family history of other affected individuals (11% of cases) Note: Mechanisms 4, 5, and 6 account for approximately 25% of cases of Angelman syndrome. Because of etiologic variability and complexity of the diagnostic process, families of children suspected of having either of these disorders should be referred for genetic evaluation and diagnostic testing to ensure the most accurate determination of etiologic mechanism, and therefore, of recurrence risk. In neonates, in addition to hypotonia, poor sucking and swallowing are common and predispose to choking episodes that can cause respiratory problems. Subsequently motor development is delayed, speech even more so, and most patients have cognitive impairment in the mild to moderate range. Hypotonia abates over the first 2 to 3 years, and patients develop an insatiable appetite that rapidly results in morbid obesity. The distribution of excess fat is particularly prominent over the lower trunk, buttocks, and proximal limb. Although the facies are not particularly dysmorphic, they are similar in most Prader-Willi patients. The bifrontal diameter is narrow, the eyes are often described as "almond shaped," and strabismus is not unusual. Hypopigmentation is common, the patient usually having blond to light brown hair, blue eyes, and sun-sensitive fair skin. Hands and feet are noticeably small from birth, and the stature of the older child and adult is short. The penis and testes are hypoplastic in males with Prader-Willi syndrome, although the penile size can be enlarged by testosterone therapy. Menarche in females is delayed or absent, and menses, when present, are sparse and irregular. Of particular concern in older children with Prader-Willi syndrome are problems of emotional lability and extreme temper tantrums. These conditions and the overeating often can be partly ameliorated by intensive inpatient behavioral modification programs followed by longitudinal parental support and follow-up in the home. Interestingly, despite a normal basal metabolic rate, weight reduction requires significantly more severe caloric restriction in these patients than in normal persons. Diabetes mellitus can develop in the older child, and its incidence is correlated with the severity of obesity. Although it tends to be insulin resistant, the condition responds well to treatment with oral hypoglycemic agents. Life expectancy can be shortened by cardiorespiratory complications related to the extreme obesity (pickwickian syndrome). Clinical Findings in Angelman Syndrome Angelman syndrome, first recognized in 1956, has an incidence of 1 in 15,000 to 1 in 20,000 live births. Except for the tendency to have hypopigmentation, the clinical phenotypes of Prader-Willi and Angelman syndromes are quite different. The latter have severe cognitive deficits, speech is impaired or absent, and inappropriate paroxysms of laughter are common. Physical features include microbrachycephaly, maxillary hypoplasia, large mouth, prognathism, and short stature (in adults). Although survival to adulthood is possible, to date only one patient with Angelman syndrome has been known to reproduce. Note the macrosomia, macroglossia, and asymmetry with hemihypertrophy and omphalocele and/or umbilical hernia. B, At 3 months old, note the macroglossia, right facial prominence, and ear creases. The latter may catalyze a step in formation or modification of another product, a step in cell metabolism, or one of a number of steps involved in the breakdown or degradation of molecules that are no longer necessary. Approximately 30,000 genes are arranged in linear fashion on the chromosomes, all having their own specific locus. Genes range in length from about a thousand to hundreds of thousands of bases in length (any of which can be subject to mutation). Exons are further subdivided into triplets of bases, termed codons, each of which encodes a specific amino acid within the polypeptide product. Because there are 64 possible triplet combinations of the four nucleotide bases (adenine, guanidine, thymine, and cytosine) and 20 amino acids, most amino acids have more than one codon that can specify them, the exceptions being methionine and tryptophan, which have only one specific codon each. After assembly, the polypeptide chain is released from its template and then may be subject to posttranslational modification. Steps may include folding, bonding into a three-dimensional conformation, being combined with another or other polypeptide chains as part of a protein complex, being split into smaller segments, and addition of phosphate or carbohydrate moieties. Thereafter, it is transported to its site of action via directional terminal sequences, which are then cleaved from the finished product. Mutation of a gene encoding the polypeptide product or for any molecule used at any step along the entire process can adversely influence the end product. Most appear to affect only one to a few to several base pairs via substitution of one base for another or by deletion or insertion of one or more bases. One example is a base substitution within a codon for an amino acid that changes it to another codon specifying the same amino acid. Still other mutations have no adverse effect but rather encode normal variations in human characteristics. The greater the degree of functional loss, the more severe the clinical manifestations of the disorder and often the earlier their onset. At 1 month the infant was admitted to "rule out sepsis" with high fever, but all the workup was negative. C, Low nasal bridge, periorbital wrinkling, full forehead, prominent lips, and prominent supraorbital ridges. The mother and her maternal female relatives have variable and milder clinical features. B Mutation(s) of gene(s) within the nuclear genome are also recognized as mendelian disorders. Phenotype/genotype correlations are unfolded by detailed clinical evaluation, recognition at a clinical level, and confirmation by molecular diagnostics confirming the genotype. Gene penetrance, disease expressivity, genetic (locus) heterogeneity, and allelic heterogeneity are some of the well-recognized complexities characterizing mendelian disorders. The latter are composed of hundreds of amino acid triplet repeats, with glycine (the smallest amino acid) being the first member of each triplet and forming the apex of each bend in the helical structure. The assembly of these may be slowed; they may be subject to excessive posttranslational modification, may be unstable and subject to degradation, or may have difficulty conforming and associating with other pro-chains to form the triple helix. The end result of this is that the patient can make only 50% of the expected amount of type I collagen, although the entire product is structurally normal. When the gene product is an enzyme or a component of an enzyme, this results in interruption of its step in a chain of reactions that may be involved in the formation or modification of a product, a step in cell metabolism, or in the degradation of molecules no longer needed by the cell. The missed step results in a build-up of substrate from the step preceding the one in which the affected enzyme acts. In others, ever-expanding storage of substrate can adversely affect cell function, as in the lysosomal storage diseases. A to C, At 7 weeks old this patient manifested erythema, and blisters on the trunk and extremities. One-third of the patients have psychomotor delays, microcephaly, and seizures, which were not observed in this patient. D, Rash replaced with hyperpigmentation on the trunk and pale hairless patches or streaks subsequently on the lower limbs. Note the down-slanted palpebral fissures, malar hypoplasia, malformed auricle, and mandibular hypoplasia. Marfan Syndrome Marfan syndrome is a genetic disorder of connective tissue that is inherited as an autosomal dominant trait, although approximately 25% to 30% of cases represent new mutations. As a result, the molecular structure of the protein fibrillin, an intrinsic component of connective tissue, is abnormal. Clinical consequences are most notable in the musculoskeletal, cardiovascular, and ocular systems and in the dura. A defect in the suspensory ligaments of the eye is responsible for subluxation of the lens (seen in 50% to 60% by 10 years old), which is usually displaced in an upward direction. Myopia and astigmatism are common, and affected individuals are also at risk for developing glaucoma, cataracts, and retinal detachment in adulthood. Mitral valve prolapse may progress to mitral insufficiency (at times associated with arrhythmias). Of great concern is progressive aneurysmal dilatation of the ascending aorta and, less commonly, the thoracic or abdominal aorta. The latter is the major source of morbidity and mortality because it can result in acute dissection and death. The incidence of hernias, both inguinal and femoral, is increased, and patients often have striae of the skin in unusual places such as the shoulder. Although most Marfan individuals are of normal intelligence, an occasional patient may have learning disabilities. In addition, family history and multiorgan manifestations are variable and may have age-dependent expressivity. All the manifestations of this condition are classified as either major or minor diagnostic criteria. The diagnostic criteria for Marfan syndrome (first established in Berlin; Beighton et al, 1988) were revised as the Ghent criteria (de Paepe et al, 1996). These have continued to be revised, and the most recent revised Ghent diagnostic criteria were established in 2010 (Loeys et al, 2010). The diagnostic criteria are based on cardiovascular, ocular, and skeletal features; the presence of a dural ectasia; and family history. These revisions have placed an increasing emphasis on the cardinal features of Marfan syndrome. Because it takes time for a number of the major abnormalities to develop or to become clinically evident, a firm diagnosis is generally impossible in early childhood, especially in the absence of a positive family history.
Multiple arteries may also increase the risk muscle relaxant gel order rumalaya gel 30 gr overnight delivery, although loss of a polar artery will not necessarily lead to graft loss muscle relaxant phase 2 block buy generic rumalaya gel line. Loss of one of the arteries is most problematic when it supplies the lower pole muscle relaxant on cns generic 30gr rumalaya gel with amex, as the risk of ureteric ischaemia and complications is increased white muscle relaxant h 115 purchase discount rumalaya gel online. It is thought that most arterial thrombosis results from damage to the intima during retrieval spasms side of head order genuine rumalaya gel, bench preparation or implantation muscle relaxant brand names buy genuine rumalaya gel line, technical failure at the anastomosis, or damage to the recipient iliac vessel. Concomitant haemodynamic changes in the recipient are also likely to contribute, as reflected by many of the other risk factors. Causes include technical failure at the anastomosis, prothrombotic conditions, and extrinsic compression from fluid collections or a haematoma. Diagnosis is made on ultrasound with an enlarged graft, absent flow in the renal vein, and reversed arterial flow in diastole. The risk of allograft thrombosis is also increased in the presence of delayed graft function (Bakir et al. Due to interstitial oedema, renal cortical flow will be sluggish leading to first venous then arterial thrombosis. When discovered, in most cases surgical rescue is not possible and transplant nephrectomy is usually required. Anaemia and perioperative bleeding Most of the blood loss following the transplantation procedure occurs at the time of organ reperfusion, that is, when the vascular clamps are released. Many patients with renal failure will have a degree of pre-existing anaemia, which compounds the effects of intraoperative blood loss. Careful bench preparation of the kidney and anastomotic technique, with adequate intraoperative attention to bleeding points will reduce the risk of haemorrhage but there will still be cases in which blood loss will require transfusion. Significant postoperative bleeding is uncommon, and can be identified by haemodynamic instability, a falling haemoglobin concentration, swelling, blood in drains, and decreased urine output related to compression. Careful removal of the packs will then allow identification of the bleeding point. Direct suture repair is sometimes possible, but in some cases re-implantation of the vessel or even explant, back table cold-perfusion and bench repair may be required for bleeding from awkward bleeding points. When re-operating for bleeding, the surgeon and theatre staff should be aware of these options and a full range of vascular clamps, along with perfusion fluids and ice, should be available. Slow venous or kidney surface bleeding can lead to gradual accumulation of a haematoma in the retroperitoneal space. This will manifest as increasing swelling, obstruction, or dysfunction due to pressure or flank bruising. Such bleeding is often related to coagulation dysfunction, which should be sought and corrected with the appropriate blood products, or reversal of anticoagulation. If there is a pressure effect or evidence of infection, the patient should be returned to theatre for exploration, evacuation of clot, and haemostasis, even though active bleeding will often have stopped. The exception is in patients requiring post-transplant dialysis for delayed-graft function, in whom anaemia often worsens. Even in those with primary function, the acute phase response to surgery, immunosuppressive drugs such as mycophenolate, azathioprine, and sirolimus can all contribute to postoperative anaemia. Early urinary complications the routine use of a ureteric stent has made early ureteric complications rare. Disruption of the ureteric anastomosis usually leads to a urinary leak, resulting in swelling, pain, and potential compression of the graft and vessels, which will cause a rise in the serum creatinine. If a retroperitoneal drain is left in the iliac fossa next to the kidney, biochemical analysis of the drain fluid will show a high creatinine concentration. Initial management will be percutaneous drainage to relieve pressure and aid diagnosis, but most patients will require surgical re-implantation. Haematuria is common in the early post-transplant period, and is usually self-limiting. Bleeding usually arises from the bladder wall at the point of ureteric insertion, but can also result from retrieval or intraoperative biopsy damage to the transplant kidney. Infection Most infections seen in the early post-transplant period are those common to any major abdominal surgical procedure, that is, involving the urinary tract, the wound, or respiratory tract. Opportunistic infections related to immunosuppression are uncommon in the early weeks. Obtaining appropriate samples for microbiological examination before starting empirical antibiotics is essential to avoid over treatment. Most transplant units have a policy of giving broad-spectrum antibiotic prophylaxis as a single perioperative dose. Others use routine postoperative prophylaxis for urinary tract infection, which may reduce the risk of sepsis but risks the development of resistant organisms (Green et al. Oral co-trimoxazole given as prophylaxis for Pneumocystis pneumonia acts as urinary tract prophylaxis in the majority of patients. Hypertension the majority of patients with renal failure will be taking one or more antihypertensive agents. With the exception of beta blockers, it is usual to stop antihypertensive medications at the time of transplantation and reintroduce them in a stepwise fashion as required in the postoperative period. Management of post-transplant hypertension is important to prevent graft damage, and to minimize cardiovascular disease. The first-choice drugs are calcium channel blockers which are effective and reduce the risk of graft loss, and improve graft function (Cross et al. Beta blockers appear safe as a second-line agent, although caution should be exercised in patients with a history of airways obstruction or peripheral vascular disease. Routine outpatient care the standard transplant surgery is now such that it is now usual for patients with primary graft function to be discharged from hospital within a week, to be reviewed regularly in dedicated discharge clinics. Such a policy requires the adequate provision of outpatient clinics, with patients being reviewed three times a week or more in the 2 weeks following transplantation. In the absence of complications, the frequency of the visits is gradually reduced to once a week by 1 month. Clinical assessment At each clinic visit, the patient should be questioned about any new issues, with particular attention paid to weight which is a good guide to fluid balance, wound complications, graft tenderness, pyrexia or other evidence of infection, and medication side effects. An up-to-date list of medications and doses should be maintained, with regular review to ensure that prophylactic drugs are stopped at appropriate time-points and medication interactions are avoided. This is best achieved by working with a dedicated transplant pharmacist in the outpatient clinic. In the early postoperative period the wound should be examined at every visit to exclude the presence of infection or swelling, and the graft should be palpated Recurrence of primary disease Recurrence of primary renal disease is an uncommon cause of early graft dysfunction (see Chapter 289). Monitoring of the urinary protein:creatinine ratio may aid early detection of recurrent disease, and the findings of significant Table 280. The signs of fluid overload include hypertension, an increase in weight, peripheral oedema and eventually signs of heart failure, including pulmonary oedema. Investigations At each clinic visit, a full set of laboratory tests including urea and electrolytes, liver function tests, calcium, phosphate, and full blood count should be requested. Routine urine samples should be tested by dip-stick for leucocytes, nitrites, blood and protein. Samples should only be sent for microbiological examination if there is evidence of infection. If proteinuria is detected, a sample should be sent for a urine protein:creatinine ratio. Frequency of screening varies, but should be once per month in the early post-transplant period. Continuing patient education the importance of patient education and instruction following transplantation should be emphasized. Understanding the restrictions placed by lifelong immunosuppression, and the risks of infection, malignant disease, and cardiovascular disease need to be sensitively explained. Many patients are concerned about the risk of infection and returning to normal activities and work following their transplant. Most patients should expect to be off work for 6 weeks, but this will vary depending on the postoperative course and the occupation. Gentle exercise should be encouraged from discharge, and activity gradually increased over the coming weeks. Patients should avoid contact with children with transmissible disease like chickenpox and parvovirus, especially if they are not immune. A healthy diet with modest salt content and sufficient calories should be encouraged. Patients must be warned about the increased risk of skin malignancy resulting from immunosuppression, and told to avoid sun exposure and encouraged to use high-factor sun cream. They should, however, be reassured that with the help of obstetric physicians, pregnancy is usually successful. Doppler ultrasound will exclude vascular and ureteric complications, as well as fluid collections causing compression. If the ultrasound is unremarkable, the essential and most informative investigation is a renal biopsy performed under ultrasound guidance. In the majority of cases this will identify the cause and differentiate between conditions requiring an increase in immunosuppression. Acute rejection Acute rejection is now very uncommon in the first week after transplantation, but can occur at any point thereafter with the highest risk seen in the first few months. Early acute rejection is typically cell mediated, and is managed with high-dose boluses of corticosteroids. After successful treatment, it is recommended that maintenance corticosteroids be administered in those patients in whom they have been previously withdrawn. Patients not receiving azathioprine or mycophenolate should be commenced on mycophenolate, Management of graft dysfunction the most important question to be decided in the outpatient clinic is whether the graft is functioning satisfactorily or whether there has been a significant deterioration. Further investigation should be triggered by an increase in serum creatinine of 10% or more over baseline. Many of these occur during the inpatient stay, but some, such as graft thrombosis and recurrence of primary disease, can occur at any point. Ureteric stenosis the routine use of ureteric stents means that most ureteric complications do not manifest until after the stent is removed, that is, up to 6 weeks following transplant. Following stent removal, a rise in serum creatinine or graft tenderness, coupled with reduced urine output, may indicate ureteric stenosis which can be confirmed by the detection of transplant hydronephrosis on ultrasound. This is explained by a compromise to the ureteric blood supply which comes from a single branch of the renal artery, which can be surgically damaged, or thrombosis because of reduced blood flow. The risk can be reduced by avoiding stripping peri-ureteric tissues and cutting short the ureter before anastomosing it to the bladder. Emergency management involves insertion of a nephrostomy to relieve calyceal pressure. This is followed by a nephrostogram to determine the site and extent of obstruction, and antegrade stent insertion as a temporary measure. Successful definitive management with balloon dilatation of the stricture at flexible nephroureteroscopy has been reported, although some patients required additional laser endoureterotomy (Kristo et al. Failure of dilatation will require surgical intervention, with the procedure of choice dictated by the site and length of the stricture. Distal strictures, especially those short in length, may be managed with simple re-implantation. Longer or more proximal strictures may require reconstruction with a psoas hitch or Boari flap, or ureteroureterostomy to the native ureter. Lymphocoele Lymphocoeles usually present as a localized swelling or tenderness over the graft site, often with graft dysfunction due to compression of the renal vein or ureter. They are caused by disruption of the lymphatics around the iliac vessels during surgical dissection. Careful surgical technique with ligation of all lymphatic vessels is essential, and since the use of electrocautery or the harmonic scalpel this complication has significantly decreased. Diagnosis is confirmed with the detection of a fluid collection on ultrasound, and biochemical analysis will demonstrate a low creatinine (excluding a urinoma) and high triglyceride content. Small, asymptomatic lymphocoeles can be managed conservatively, but larger collections will require intervention. Whilst percutaneous drainage may be successful, the risk of infection and recurrence means that laparoscopic fenestration to the peritoneal cavity is preferred (Lucewicz et al. Risk factors for late stenosis include increasing recipient and donor age, extended criteria donors, delayed graft function, and recipient ischaemic heart disease. Initial investigation is by Doppler ultrasound if an appropriately trained sonographer is available, but more usually by computed tomography or magnetic resonance angiogram. If there is doubt as to the significance of a stenosis, formal angiography with pressure measurement can be used; a drop of > 20 mmHg suggests significant stenosis. These include arterial dissection and rupture, thromboembolism, and puncture site complications. Routine screening or investigation of graft dysfunction will identify the presence of decoy cells in the urine. Delayed graft function: risk factors and the relative effects of early function and acute rejection on long-term survival in cadaveric renal transplantation. Effectiveness of a 5-day external stenting protocol on urological complications after renal transplantation. Effect of perioperative blood transfusions on long term graft outcomes in renal transplant patients. Pre-emptive treatment for cytomegalovirus viraemia to prevent cytomegalovirus disease in solid organ transplant recipients.
Donor-specific antibodies accelerate arteriosclerosis after kidney transplantation muscle relaxant drugs over the counter cheap rumalaya gel uk. Functionally significant renal allograft rejection is defined by transcriptional criteria muscle relaxant phase 2 block buy rumalaya gel no prescription. Histological chronic allograft damage index accurately predicts chronic renal allograft rejection spasms shown in mri purchase rumalaya gel 30 gr overnight delivery. Molecular correlates of scarring in kidney transplants: the emergence of mast cell transcripts muscle relaxant in anesthesia buy cheap rumalaya gel 30gr. Microarray analysis of rejection in human kidney transplants using pathogenesis-based transcript sets spasms near liver discount 30gr rumalaya gel free shipping. Dense B cell infiltrates in paediatric renal transplant biopsies are predictive of allograft loss muscle relaxant drugs buy rumalaya gel 30gr mastercard. Serine proteinase inhibitor-9, an endogenous blocker of granzyme B/perforin lytic pathway, is hyperexpressed during acute rejection of renal allografts. Tacrolimus exposure and evolution of renal allograft histology in the first year after transplantation. Detection of subclinical tubular injury after renal transplantation: comparison of urine protein analysis with allograft histopathology. Proteomic-based identification of cleaved urinary beta2-microglobulin as a potential marker for acute tubular injury in renal allografts. B cells in cluster or in a scattered pattern do not correlate with clinical outcome of renal allograft rejection. Serial peripheral blood perforin and granzyme B gene expression measurements for prediction of acute rejection in kidney graft recipients. Banff `09 meeting report: antibody mediated graft deterioration and implementation of Banff working groups. Detectable circulating antiendothelial cell antibodies in renal allograft recipients with C4d-positive acute rejection: a report of three cases. Cytotoxic lymphocyte gene expression in peripheral blood leukocytes correlates with rejecting renal allografts. Comparison between bortezomib and rituximab in the treatment of antibody-mediated renal allograft rejection. Transplant glomerulopathy: ultrastructural abnormalities occur early in longitudinal analysis of protocol biopsies. Urinary cytotoxic molecular markers for a noninvasive diagnosis in acute renal transplant rejection. In general, the intensity of immunosuppression is at its highest for a year after solid organ transplant (Jong and Freedman, 2012). Guidelines on diagnosis, treatment, and prevention of many infections after solid organ transplant have been provided by the Infectious Diseases Community of Practice of the American Society of Transplantation (2013). In the first month after organ transplant, infections tend to be related to the surgical procedure and hospital environment, and include wound infection, consequences of anastomotic leaks and ischaemia, aspiration pneumonia, catheter infection, and Clostridium difficile colitis. Donor-derived infections and recipient-derived infections, due to prior colonization with agents such as Aspergillus or Pseudomonas, may present in this phase. Their risk can be mitigated or delayed by prophylaxis, and increased by intensified immunosuppression, leucopenia, or immunomodulatory viral infections. The stable and relatively healthy organ transplant recipient who is > 6 months out from transplant tends to develop community-acquired or ordinary infections, including urinary tract infections, upper respiratory infections and pneumonia, gastroenteritis, and varicella zoster. Infections with unusual and opportunistic pathogens such as Aspergillus, unusual moulds, Nocardia. Pre-transplant evaluation can mitigate the risk of some infections, especially latent ones. Potential transplant recipients and donors are screened for latent tuberculosis, by history, chest X-ray, skin testing, or use of an interferon gamma release assay-based blood test such as the T. Recipients from or in endemic regions should be screened for latent infections such as T. Those subjects seronegative for measles, mumps, rubella, hepatitis A and B, and varicella should be vaccinated pre transplant. Some vaccines are live so cannot be given after transplant when the recipient is immunosuppressed (Jong and Freedman, 2012). For example, transplant recipients infected with West Nile virus are much more likely to have clinical illness and succumb. Clinicians need to consider a broad differential diagnosis in transplant recipients. The diagnosis of emerging, novel, and atypical pathogens is especially challenging in this vulnerable population, as has been seen with cases of lymphocytic choriomeningitis virus, tuberculosis, Chagas disease, and strongyloidiasis. Such infection occurs in up to 1% of deceased donor organ transplants (Ison and Nalesnik, 2011). Such unanticipated donor-derived infections range from viruses such as rabies, lymphocytic choriomeningitis and West Nile virus, to bacteria including tuberculosis, fungi including cryptococcosis and histoplasmosis, and parasites such as Trypanosoma cruzi (causing Chagas disease) and Strongyloides stercoralis (Ison and Nalesnik, 2011). Enhanced appreciation of donor-derived infections has resulted in better screening and diagnosis. Infections tend to occur in fairly predictable phases after solid organ transplant. While many of the classic opportunistic infections occur in the first six months, the period of most intense immunosuppression, the risk of such infection is indefinite and still exists for a period after discontinuation of immunosuppressive drugs. The risk of infection is decreased by the use of prophylaxis, and increased by the use of more potent immunosuppression (both in the induction and maintenance phases, and after treatment of rejection), allograft rejection itself, concomitant infections, leucopenia, and technical complications of surgery. Viruses: prophylaxis, diagnosis, and management Viruses are the most common cause of infection after transplantation. Viruses of the human herpes virus family are the most common viral pathogens after transplantation. Disseminated infection from any of the human herpes viruses can be life-threatening. Recipients who acquire de novo infection from their donors, who do not have prior immunity to these viruses, are at highest risk for severe infection. Hepatitis viruses (primarily B and C) are common reasons for liver transplantation and commonly complicate transplantation, predominantly as reactivation of latent infections. The primarily zoonotic hepatitis E has been reported as an emerging pathogen in transplant recipients. Numerous other viruses have been shown to cause disease in transplant recipients, including parvovirus B19, West Nile virus, and lymphocytic choriomeningitis. These outcomes fall somewhere in the national database between kidney transplant recipients who are > 65 years old and those reported for all kidney transplant recipients. Multivariate analysis showed that the risk of graft loss was increased among patients treated for rejection and those receiving antithymocyte globulin induction therapy, while living-donor transplants were protective. A higher-than-expected rejection rate was observed, with 1-year and 3-year estimates of 31% and 41%, respectively. Disadvantages include lower rates of graft and patient survival, higher rates of opportunistic infections, and more complex logistics (organizing and managing the results of weekly testing for several months after transplant). Institutions should develop local protocols, based on clinical outcomes, use of cytolytic induction therapies, the overall state of immunosuppression, costs, and ability to do periodic testing. Compelling data comes from a randomized clinical trial of valganciclovir prophylaxis (N = 74) versus pre-emptive therapy with intravenous ganciclovir (N = 74). Prophylaxis significantly improved long-term graft survival 4 years after transplant (92. Costs of serial testing (including personnel and laboratory costs) may be similar to the costs of medications. It is, however, better to focus on long-term outcomes and overall cost and benefit to the patient and to the programme. Universal prophylaxis incurred $1464 more direct costs compared with pre-emptive therapy, while saving $7309 in indirect costs, and resulted in a net gain of 0. Thus, universal prophylaxis resulted in a cost saving of $27,967 for one quality-adjusted life year gained when compared with pre-emptive therapy. Prophylaxis Viral infections can be prevented by the use of antiviral drugs, prudent use of immunosuppression, administration of immunoglobulins, careful monitoring, and vaccination. Prophylaxis against hepatitis C is not usually given, because toxicity outweighs the benefit. Universal prophylaxis involves giving antiviral medication at prophylactic doses for a defined period of time to a cohort. Pre-emptive therapy is defined as use of treatment dose antivirals only once a certain test threshold is achieved. Although large, randomized trials have not been conducted, numerous studies suggest that universal prophylaxis results in better outcomes than those achieved with pre-emptive therapy, especially in the higher risk D+/R- population (Kotton et al. Ganciclovir only works in the very small percentage of virus that is in the lytic phase. The 10-year analysis revealed the 200-day prophylaxis as cost saving with a 2380 quality-adjusted life year gain (per 10,000 patients) and simultaneously lower cost. Miscellaneous Mosquito-borne infections such as West Nile virus, dengue fever, eastern equine encephalitis, chikungunya, and others can cause significant disease in transplant recipients. Avoidance of insect bites by wearing protective clothing, using insect repellent, and screens or sleeping nets will decrease the risk of transmission. Vaccination against influenza, hepatitis A and B, human papillomavirus, varicella zoster, and other viral pathogens can provide protection. This is best given prior to transplant, as the immunologic response is likely to be augmented. Certain viral vaccines have live attenuated virus and cannot be used after transplant, such as varicella zoster, measles, mumps, rubella, and yellow fever. In general, transplant centres are much more inclined to administer vaccines to transplant patients than previously, and influenza vaccine is recommended by numerous experts (Kumar et al. Surveys in 1999 and 2009 of United Network for Organ Sharing-certified kidney and kidney-pancreas transplant centres in the United States regarding their influenza vaccination practices established that the 2009 respondents, compared with 1999, were more likely to recommend vaccination for kidney (94. While there has been some concern that vaccines could disrupt tolerance or increase the risk of rejection, this has not so far been borne out in trials. When possible, it is recommended that transplant recipients avoid the adjuvants in some vaccines, and be given vaccines without adjuvants, which are immunostimulatory molecules (Kumar et al. The primary method of prevention is screening, and the primary method of treatment is reduction in immunosuppression. Antiviral therapy, including cidofovir and leflunomide, has an uncertain effect with significant toxicity. Diagnosis Viral infection diagnosis has been improved hugely by the availability of molecular techniques. Within a matter of hours, various amplification methods can precisely identify active replicating viral infections. In general, serology is much less helpful in the immunosuppressed population, as they are much less likely to seroconvert in response to the acute illness, and molecular diagnostics have a much higher yield. Hepatitis B Hepatitis B is a common cause of cirrhosis and the need for liver transplant. Post-transplant management may include antiviral agents such as lamivudine, entecavir, adefovir, and others, as well as the use of hyperimmune hepatitis B globulin. Other organ transplant recipients may have latent hepatitis B, which can reactivate after induction of immunosuppression, especially in those who have hepatitis B surface antigen, and much less commonly in those who have a negative surface antigen but a positive core antibody. If they are non-immune, all patients undergoing dialysis who are candidates for organ transplantation should undergo vaccination in the pre-transplant period. Some patients may need a higher dose of vaccine, and accelerated vaccine series especially if they will be undergoing organ transplantation soon. Chemoprophylaxis is encouraged for those with latent tuberculosis, or who may have exposure via their donor (Morris et al. Vaccination against Streptococcus pneumoniae, Clostridium tetani (tetanus), Corynebacterium diphtheriae, Bordetella pertussis (whooping cough), and other bacterial pathogens will provide some additional protection. Reducing the intensity of immunosuppression (even transiently) may allow for more rapid clearance of a viral infection. Although not well evidence-based, repleting recipients who have hypogammaglobulinaemia with intravenous immunoglobulin may help clear infection. To optimize the diagnostic yield of cultures, clinicians should notify the laboratory when unusual organisms are suspected, such as Listeria, Rhodococcus, mycobacteria, and Nocardia. Expanding the standard panel of antibiotic sensitivity at the time of initial diagnosis may help with subsequent therapy, especially given the increased risk of drug interactions and side effects, partly due to concomitant use of multiple medications. Serologic techniques tend to yield diagnoses less frequently in this population due to more muted immunologic responses. Management Treatment in febrile or ill transplant recipients is with empiric antibacterial therapy, which should be chosen based on local epidemiology. This approach is justified by the significant incidence of bacteraemia in the post-transplant period and by the concomitant high mortality rate when treatment is delayed. Transplant patients are at higher risk for resistant pathogens, and the empiric antibiotic choice should reflect this. Once a culture diagnosis has been made and antibiotic sensitivities are available, the antibiotic regimen may be modified. Optimal duration of therapy has usually not been well studied in this population, but is often longer than in normal hosts. Certain antibiotic classes should be avoided when possible due to toxicities and side effects. Examples include aminoglycosides (which can increase the risk of renal toxicity) and rifamycins (rifampin/rifampicin or rifabutin, which have profound interactions with tacrolimus and ciclosporin). Because of the increased rates of resistance resulting in decreased susceptibility to oral antibiotics, intravenous therapy is often needed in this population. In general, arm veins should be avoided to preserve them for future haemodialysis access in those at higher risk for chronic kidney disease.
For future pre-clinical studies muscle relaxant vicodin discount rumalaya gel 30gr with mastercard, there is a need to use experimental models that better mimic human disease yet in a timely manner spasms hands and feet rumalaya gel 30 gr otc. Reversible renal failure associated with angiotensin-converting enzyme inhibitors in polycystic kidney disease muscle relaxant medications back pain best 30gr rumalaya gel. Renal structure in early autosomal dominant polycystic kidney disease: the Consortium of Radiological Imaging Studies of Polycystic Kidney Disease muscle relaxant on cns buy discount rumalaya gel 30gr line. Embolization of polycystic kidneys as an alternative to nephrectomy before renal transplantation: a pilot study spasms falling asleep buy rumalaya gel 30 gr with visa. Intensive hemodialysis: normalizing the "unphysiology" of conventional hemodialysis The value of unenhanced helical computerized tomography in the management of acute flank pain muscle relaxant withdrawal symptoms purchase rumalaya gel online. Hypertension in autosomal dominant polycystic kidney disease: early occurrence and unique aspects. Trimethoprim-sulfamethoxazole in cyst fluid from autosomal dominant polycystic kidneys. Young women with polycystic liver disease respond best to somatostatin analogues: a pooled analysis of individual patient data. However, given that tolvaptan treatment is expected to be expensive it is currently unclear on how best to maximize its clinical benefits. Polycystic kidney disease at end-stage renal disease in the United States: patient characteristics and survival. Percutaneous nephrolithotomy for management of upper urinary tract calculi in patients with autosomal dominant polycystic kidney disease. Increased incidence of gastrointestinal surgical complications in renal transplant recipients with polycystic kidney disease. Differences in hormonal and renal vascular responses between normotensive patients with autosomal dominant polycystic kidney disease and unaffected family members. The effect of caffeine on renal epithelial cells from autosomal dominant polycystic kidney disease. Is peritoneal dialysis a suitable renal replacement therapy in autosomal dominant polycystic kidney disease. Lillian Jean Kaplan International Prize for advancement in the understanding of polycystic kidney disease. Polycystic kidney disease is a risk factor for new-onset diabetes after transplantation. Renal, cardiovascular and hormonal characteristics of young adults with autosomal dominant polycystic kidney disease. Randomized clinical trial of long-acting somatostatin for autosomal dominant polycystic kidney disease. Progressive risk, urinary protein excretion, and treatment effects of angiotensin-converting enzyme inhibitors in non-diabetic kidney disease. Long-term outcome of patients with autosomal dominant polycystic kidney disease receiving peritoneal dialysis. Triptolide is a traditional Chinese medicine-derived inhibitor of polycystic kidney disease. Peritoneal dialysis as the first-line renal replacement therapy in patients with autosomal dominant polycystic kidney disease. Inhibition of glucosylceramide accumulation results in effective blockade of polycystic kidney disease in mouse models. Evaluation of nephrolithiasis in autosomal dominant polycystic kidney disease patients. A "two-hit" model of cystogenesis in autosomal dominant polycystic kidney disease Survival after end-stage renal disease in autosomal dominant polycystic kidney disease: contribution of extrarenal complications to mortality. Risk of intracranial aneurysm bleeding in autosomal-dominant polycystic kidney disease. Identification of gene mutations in autosomal dominant polycystic kidney disease through targeted resequencing. Renal contraction therapy for enlarged polycystic kidneys by transcatheter arterial embolization in hemodialysis patients. Calcium restores a normal proliferative phenotype in human polycystic kidney disease epithelial cells. Polycystin-dependent fluid flow sensing targets histone deacetylase 5 to prevent the development of renal cysts. Additional associated vascular abnormalities include dolichoectasias, thoracic aortic and cervicocephalic artery dissections, and coronary artery aneurysms. Just as in the general population, 85% of them are found in the anterior circulation (Irazabal et al. The 1-year mortality and combined mortality-morbidity rates for surgical and endovascular repair were 2. Elimination of tobacco use and aggressive treatment of hypertension are strongly recommended. Recurrence of intracranial aneurysms in autosomal-dominant polycystic kidney disease. Familial clustering of ruptured intracranial aneurysms in autosomal dominant polycystic kidney disease. Cardiovascular polycystins: insights from autosomal dominant polycystic kidney disease and transgenic animal models. Clinical lessons and risk factors from 403 fatal cases of subarachnoid haemorrhage. Extended follow-up of unruptured intracranial aneurysms detected by presymptomatic screening in patients with autosomal dominant polycystic kidney disease. A mathematical model of utility for single screening of asymptomatic unruptured intracranial aneurysms at the age of 50 years. Repeat imaging for intracranial aneurysms in patients with autosomal dominant polycystic kidney disease with initially negative studies: a prospective ten-year follow-up. Sensitivity analyses were performed to determine the effects of altering various factors on outcomes. Additional acceptable indications are preparation for major elective surgery, high-risk occupations. There is little to be gained from screening after the age of 65 since remaining life expectancy is insufficient to see benefit (Li et al. Practical aspects of screening Screening is preferably performed by high-resolution, threedimensional, time-of-flight magnetic resonance imaging; it can be done without gadolinium allowing patients with a low glomerular filtration rate to be screened. Strategically located cysts may cause hepatic venous outflow obstruction or compression of the portal or inferior caval vein. In addition, bile duct compression may lead to obstructive jaundice (Dmitrewski et al. The disease typically becomes symptomatic in the fourth decade of life (Everson et al. Gender is the most defining risk factor for growth of hepatic cysts (Chapman, 2003). Although men and women have equal lifetime risk, females develop larger and greater numbers of hepatic cysts (Gabow et al. Indeed, female sex hormones are an established risk factor as patients who use exogenous oestrogens and have had multiple pregnancies are more severely affected (Gabow et al. Other risk factors include degree of renal dysfunction, severity of renal disease, and renal cyst volume (Gabow et al. In addition, local experience and available expertise determines which procedure is best suitable. Compression of adjacent abdominal and thoracic organs may lead to abdominal pain, abdominal distention, early satiety, shortness of breath, nausea, and vomiting (Doty and Tompkins, 1989; Vauthey et al. Complications of cysts are uncommon and typically occur in severe Radiological management Aspiration-sclerotherapy is the preferential treatment for a dominant and large, likely symptomatic, superficially located cyst. With the procedure, one or several cysts are punctured under radiological guidance, and aspirated to ensure complete fluid evacuation (van Keimpema et al. A sclerosant is injected to destroy the epithelial lining curtailing fluid production (Saini et al. Ethanol is most commonly used, but minocycline and tetracycline are alternatives (Tokunaga et al. Cysts recur in approximately 20% of treated patients, and in these cases, multiple sessions may be needed (Drenth et al. Surgical management Surgical options for treatment of polycystic livers include fenestration, segmental hepatic resection, and liver transplantation. Fenestration is a technique that combines aspiration and surgical deroofing of multiple cysts in a single procedure to achieve volume reduction (Russell and Pinson, 2007). The main indication for fenestration is a patient with multiple liver cysts (> 4 cm) accessible by laparotomy or laparoscopy (van Keimpema et al. Although immediate symptom relieve is achieved in 92% of cases, recurrence of symptoms (22%) and cysts (24%) occur (Drenth et al. Complications of fenestration occur in approximately 23% and include ascites, pleural effusion, arterial or venous bleeding, and biliary leakage (van Keimpema et al. Laparoscopy leads to a lower complication rate (29% vs 40%) and is therefore preferred over laparotomy (Martin et al. The main disadvantage of a laparoscopic approach is that cranially located liver cysts are difficult to reach. Segmental hepatic resection is considered in severe symptomatic patients with cyst-rich liver segments and at least one predominantly normal liver segment. The procedure is often combined with fenestration for deroofing of cysts in the remnant segment (Russell and Pinson, 2007). The distribution of cysts in the liver dictates the extension of the resection, although at least 25% normal liver parenchyma must be present to have a beneficial postresectional outcome (Schindl et al. However, the procedure is associated with considerable morbidity (51%) and mortality (3%) (Drenth et al. Furthermore, the risk of subsequent adhesions may complicate a possible future liver transplantation (Starzl et al. Candidates for liver transplantation are patients with extremely impaired quality of life or with untreatable complications such as portal hypertension and nutritional compromise (Russell and Pinson, 2007). The overall morbidity after liver or combined liver-kidney transplantation is 41%, but with time, 91% of patients report improved quality of life (Kirchner et al. In these cases, a liver and kidney from the same donor is preferable, as it protects the kidney graft from rejection and improves kidney graft survival (Shaked et al. These observations suggest that somatostatin analogues affect the natural course of the disease. The most important question to address in future studies is whether this beneficial effect is maintained with prolonged therapy. Although the effect of sirolimus on polycystic liver volume is impressive, formal randomized trials need to confirm this observation. How to select a treatment greatly depends on localization and size of cysts and we suggest an algorithm to facilitate the choice of therapy. New advances in evaluation and management of patients with polycystic liver disease. Liver involvement in autosomal-dominant polycystic kidney disease: therapeutic dilemma. Adult polycystic liver disease: is fenestration the most adequate operation for long-term management Hepatic and renal manifestations in autosomal dominant polycystic kidney disease: a dichotomy of two ends of a spectrum. Hepatic cystic disease in an adult polycystic kidney disease transplant population. Outcome and quality of life in patients with polycystic liver disease after liver or combined liver-kidney transplantation. Liver resection and cyst fenestration in the treatment of severe polycystic liver disease. Combined transplantation of liver and kidney from the same donor protects the kidney from rejection and improves kidney graft survival. The role of combined liver/kidney transplantation in end-stage hepato-renal disease. Lanreotide reduces the volume of polycystic liver: a randomized, double-blind, placebo-controlled trial. Laparoscopic fenestration of liver cysts in polycystic liver disease results in a median volume reduction of 12. Treatment of symptomatic hepatic cysts by percutaneous instillation of minocycline hydrochloride. First case report of percutaneous drainage and sclerosis with doxycycline, with a review of literature. Aspiration-sclerotherapy results in effective control of liver volume in patients with liver cysts. Bear and colleagues proposed a rate of false negative ultrasonographic diagnosis of about 35% below the age of 10 years (Bear et al. Where an earlier diagnosis is essential, magnetic resonance imaging is more sensitive than ultrasound (see Chapter 308), but if a positive genetic diagnosis has been made in the family, genetic testing is likely to be definitive. Families with early-manifesting offspring have a high recurrence risk of almost 50% for the birth of a child with a similar clinical course (Zerres et al. Increased risk extends also to offspring of affected siblings of the respective parent carrying the same germline mutation (Ross and Travers, 1975; Gal et al. Conclusive data of underlying mechanisms are still lacking and a matter of ongoing research. Most seriously discussed mechanisms are anticipation, imprinting, and the segregation of modifying genes. Anticipation denotes the progressively earlier appearance and increased severity of a disorder in successive generations. Furthermore, several groups failed to find any evidence of anticipation (Geberth et al.
Rumalaya gel 30gr on line. Egypt Muscle 2013 - Big Ramy is posing.


















