Nexium

Jonathan Abrams, MD
- Distinguished Professor of Medicine
- University of New Mexico
- Cardiology Division
- Albuquerque, New Mexico
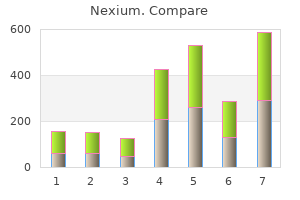
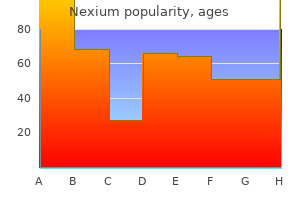
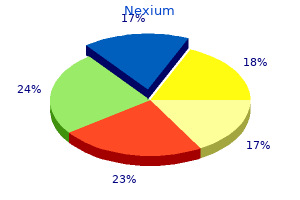
Other prominent features include hyperactivity gastritis diet watermelon nexium 20mg lowest price, nervousness gastritis kronik aktif adalah purchase generic nexium on line, and irritability gastritis gallbladder removal purchase nexium 20 mg on line, ultimately leading to a sense of easy fatigability in some patients gastritis ulcer buy cheap nexium 20 mg on-line. Insomnia and impaired concentration are common; apathetic thyrotoxicosis may be mistaken for depression in the elderly gastritis kombucha buy cheap nexium 40mg on line. Fine tremor is a frequent finding gastritis diet ���� buy line nexium, best elicited by having patients stretch out their fingers while feeling the fingertips with the palm. Common neurologic manifestations include hyperreflexia, muscle wasting, and proximal myopathy without fasciculation. Thyrotoxicosis is sometimes associated with a form of hypokalemic periodic paralysis; this disorder is particularly common in Asian males with thyrotoxicosis, but it occurs in other ethnic groups as well. The most common cardiovascular manifestation is sinus tachycardia, often associated with palpitations, occasionally caused by supraventricular tachycardia. The high cardiac output produces a bounding pulse, widened pulse pressure, and an aortic systolic murmur and can lead to worsening of angina or heart failure in the elderly or those with preexisting heart disease. Treatment of the thyrotoxic state alone converts atrial fibrillation to normal sinus rhythm in about half of patients, suggesting the existence of an underlying cardiac problem in the remainder. The skin is usually warm and moist, and the patient may complain of sweating and heat intolerance, particularly during warm weather. Palmar erythema, onycholysis, and, less commonly, pruritus, urticaria, and diffuse hyperpigmentation may be evident. Hair texture may become fine, and a diffuse alopecia occurs in up to 40% of patients, persisting for months after restoration of euthyroidism. Gastrointestinal transit time is decreased, leading to increased stool frequency, often with diarrhea and occasionally mild steatorrhea. Women frequently experience oligomenorrhea or amenorrhea; in men, there may be impaired sexual function and, rarely, gynecomastia. The direct effect of thyroid hormones on bone resorption leads to osteopenia in long-standing thyrotoxicosis; mild hypercalcemia occurs in up to 20% of patients, but hypercalciuria is more common. There is a small increase in fracture rate in patients with a previous history of thyrotoxicosis. There may be a thrill or bruit, best detected at the inferolateral margins of the thyroid lobes, due to the increased vascularity of the gland and the hyperdynamic circulation. Lid retraction, causing a staring appearance, can occur in any form of thyrotoxicosis and is the result of sympathetic overactivity. This condition is also called thyroid-associated ophthalmopathy, because it occurs in the absence of hyperthyroidism in 10% of patients. The earliest manifestations of ophthalmopathy are usually a sensation of grittiness, eye discomfort, and excess tearing. About one-third of patients have proptosis, best detected by visualization of the sclera between the lower border of the iris and the lower eyelid, with the eyes in the primary position. In severe cases, proptosis may cause corneal exposure and damage, especially if the lids fail to close during sleep. Although most frequent over the anterior and lateral aspects of the lower leg (hence the term pretibial myxedema), skin changes can occur at other sites, particularly after trauma. The typical lesion is a noninflamed, indurated plaque with a deep pink or purple color and an "orange skin" appearance. Nodular involvement can occur, and the condition can rarely extend over the whole lower leg and foot, mimicking elephantiasis. The converse state of T4 toxicosis, with elevated total and unbound T4 and normal T3 levels, is occasionally seen when hyperthyroidism is induced by excess iodine, providing surplus substrate for thyroid hormone synthesis. Associated abnormalities that may cause diagnostic confusion in thyrotoxicosis include elevation of bilirubin, liver enzymes, and ferritin. Clinical features of thyrotoxicosis can mimic certain aspects of other disorders, including panic attacks, mania, pheochromocytoma, and weight loss associated with malignancy. The clinical course of ophthalmopathy does not follow that of the thyroid disease, although thyroid dysfunction can worsen eye signs. However, the course is more fulminant in up to 5% of patients, requiring intervention in the acute phase if there is optic nerve compression or corneal ulceration. Diplopia may appear late in the disease due to fibrosis of the extraocular muscles. Radioiodine treatment for hyperthyroidism worsens the eye disease in a small proportion of patients (especially smokers). Antithyroid drugs or surgery have no adverse effects on the clinical course of ophthalmopathy. Antithyroid drugs are the predominant therapy in many centers in Europe, Latin America, and Japan, whereas radioiodine is more often the first line of treatment in North America. These 2706 differences reflect the fact that no single approach is optimal and that patients may require multiple treatments to achieve remission. The main antithyroid drugs are thionamides; propylthiouracil, carbimazole (not available in the United States), and the active metabolite of the latter, methimazole. These drugs also reduce thyroid antibody levels by mechanisms that remain unclear, and they appear to enhance spontaneous rates of remission. However, this effect is of minor benefit, except in the most severe thyrotoxicosis, and is offset by the much shorter half-life of this drug (90 min) compared to methimazole (6 h). The starting dose of an antithyroid drug can be gradually reduced (titration regimen) as thyrotoxicosis improves. Less commonly, high doses may be given combined with levothyroxine supplementation (block-replace regimen) to avoid drug-induced hypothyroidism. The titration regimen is preferred to minimize the dose of antithyroid drug and provide an index of treatment response. The usual daily maintenance doses of antithyroid drugs in the titration regimen are 2. In the block-replace regimen, the initial dose of antithyroid drug is held constant, and the dose of levothyroxine is adjusted to maintain normal unbound T4 levels. For unclear reasons, remission rates appear to vary in different geographic regions. Younger patients, males, smokers, and patients with a history of allergy, severe hyperthyroidism or large goiters are most likely to relapse when treatment stops, but outcomes are difficult to predict. All patients should be followed closely for relapse during the first year after treatment and at least annually thereafter. These may resolve spontaneously or after substituting an alternative antithyroid drug; rashes may respond to an antihistamine. Rare but major side effects include hepatitis (especially with propylthiouracil; avoid use in children) and cholestasis (methimazole and carbimazole); vasculitis; and, most important, agranulocytosis (<1%). It is essential that antithyroid drugs are stopped and not restarted if a patient develops major side effects. Written instructions should be provided regarding the symptoms of possible agranulocytosis. It is not useful to monitor blood counts prospectively, because the onset of agranulocytosis is idiosyncratic and abrupt. Beta blockers are also useful in patients with thyrotoxic periodic paralysis, pending correction of thyrotoxicosis. In consultation with a cardiologist, anticoagulation with warfarin should be considered in all patients with atrial fibrillation; there is often spontaneous reversion to sinus rhythm with control of hyperthyroidism, and long-term anticoagulation is not usually needed. Radioiodine causes progressive destruction of thyroid cells and can be used as initial treatment or for relapses after a trial of antithyroid drugs. There is a small risk of thyrotoxic crisis (see below) after radioiodine, which can be minimized by pretreatment with antithyroid drugs for at least a month before treatment. Antecedent treatment with an antithyroid drug and a beta blocker should be considered for all elderly patients or for those with cardiac problems. Propylthiouracil appears to have a prolonged radioprotective effect and should be stopped for a longer period before radioiodine is given, or a larger dose of radioiodine will be necessary. Efforts to calculate an optimal dose of radioiodine that achieves euthyroidism without a high incidence of relapse or progression to hypothyroidism have not been successful. Some patients inevitably relapse after a single dose because the biologic effects of radiation vary between individuals, and hypothyroidism cannot be uniformly avoided even using accurate dosimetry. A practical strategy is to give a fixed dose based on clinical features, such as the severity of thyrotoxicosis, the size of the goiter (increases the dose needed), and the level of radioiodine uptake (decreases the dose needed). Certain radiation safety precautions are necessary in the first few days after radioiodine treatment, but the exact guidelines vary depending on local protocols. For this reason, -adrenergic blockers or antithyroid drugs can be used to control symptoms during this interval. Persistent hyperthyroidism can be treated with a second dose of radioiodine, usually 6 months after the first dose. Patients should be informed of this possibility before treatment and require close follow-up during the first year followed by annual thyroid function testing. Pregnancy and breast-feeding are absolute contraindications to radioiodine treatment, but patients can conceive safely 6 months after treatment. The overall risk of cancer after radioiodine treatment in adults is not increased. Although many physicians avoid radioiodine in children and adolescents because of the theoretical risks of malignancy, emerging evidence suggests that radioiodine can be used safely in older children. Some experts recommend surgery in young individuals, particularly when the goiter is very large. The major complications of surgery-bleeding, laryngeal edema, hypoparathyroidism, and damage to the recurrent laryngeal nerves-are unusual when the procedure is performed by highly experienced surgeons. Recurrence rates in the best series are <2%, but the rate of hypothyroidism is similar to that following radioiodine treatment, especially with the current trend away from subtotal thyroidectomy. Because transplacental passage of these drugs may produce fetal hypothyroidism and goiter if the maternal dose is excessive, maternal antithyroid dose titration should target serum free or total T4 levels at or just above the pregnancy reference range. Following cessation, careful monitoring of maternal thyroid function tests is essential. Nonetheless, the transplacental transfer of these antibodies if present at levels 3 times higher than the normative range rarely causes fetal or neonatal thyrotoxicosis. Thyrotoxic crisis, or thyroid storm, is rare and presents as a life-threatening exacerbation of hyperthyroidism, accompanied by fever, delirium, seizures, coma, vomiting, diarrhea, and jaundice. The mortality rate due to cardiac failure, arrhythmia, or hyperthermia is as high as 30%, even with treatment. Management requires intensive monitoring and supportive care, identification and treatment of the precipitating cause, and measures that reduce thyroid hormone synthesis. Although other -adrenergic blockers can be used, high doses of propranolol decrease T4 T3 conversion, and the doses can be easily adjusted. Caution is needed to avoid acute negative inotropic effects, but controlling the heart rate is important, as some patients develop a form of highoutput heart failure. Ophthalmopathy requires no active treatment when it is mild or moderate, because there is usually spontaneous improvement. General measures include meticulous control of thyroid hormone levels, cessation of smoking, and an explanation of the natural history of ophthalmopathy. Corneal exposure during sleep can be avoided by using patches or taping the eyelids shut. Severe ophthalmopathy, with optic nerve involvement or chemosis resulting in corneal damage, is an emergency requiring joint management with an ophthalmologist. When glucocorticoids are ineffective, orbital decompression can be achieved by removing bone from any wall of the orbit, thereby allowing displacement of fat and swollen extraocular muscles. The transantral route is used most often because it requires no external incision. Proptosis recedes an average of 5 mm, but there may be residual or even worsened diplopia.

If the patient has a sexual partner gastritis symptoms mayo nexium 20 mg overnight delivery, the partner should be included in counseling because of the dramatic physical and sexual changes that occur with androgen treatment gastritis and bloating order cheap nexium on line. Contraindications for Androgen Administration Testosterone administration is contraindicated in men with prostate or breast cancer (Table 384-4) gastritis diet ������� buy 40mg nexium. Testosterone therapy should not be administered without further urologic evaluation to men with a palpable prostate nodule or induration chronic gastritis of the stomach cheap nexium 40mg free shipping, or prostate-specific antigen >3 ng/mL gastritis lipase discount nexium 40mg overnight delivery, or with severe lower urinary tract symptoms (American Urological Association lower urinary tract symptom score >19) gastritis diet 8 hour order cheapest nexium and nexium. Testosterone replacement should not be administered to men with baseline hematocrit 50%, severe untreated obstructive sleep apnea, uncontrolled or poorly controlled congestive heart failure, or to men with myocardial infarction, stroke, or acute coronary syndrome in the preceding 3 months. Source: Reproduced from the Endocrine Society Guideline for Testosterone Therapy of Androgen Deficiency Syndromes in Men (Bhasin S et al: J Clin Endocrinol Metab 95:2536, 2010). Potential adverse effects include acne, oiliness of skin, erythrocytosis, breast tenderness and enlargement, leg edema, and increased risk of detection of prostate events. In addition, there may be formulation-specific adverse effects such as skin irritation with transdermal patch; risk of gel transfer to a sexual partner with testosterone gels; buccal ulceration and gum problems with buccal testosterone; pain and mood fluctuation with injectable testosterone esters; cough and injection site pain with long-acting testosterone undecanoate; and, nasal irritation, epistaxis, and nasal scab with intranasal formulation. Hemoglobin Levels Administration of testosterone to androgendeficient men is typically associated with a ~3% increase in hemoglobin levels, due to increased erythropoiesis, stimulation of erythropoietin, suppression of hepcidin, and increased iron availability for erythropoiesis. The magnitude of hemoglobin increase during testosterone therapy is greater in older men than younger men, and in men who have sleep apnea, a significant smoking history, or chronic obstructive lung disease, or who live at high altitude. The frequency of erythrocytosis is higher in hypogonadal men treated with injectable testosterone esters than in those treated with transdermal formulations, presumably due to the higher testosterone dose delivered by the typical regimens of testosterone esters. Erythrocytosis is the most frequent adverse event reported in testosterone trials in middle-aged and older men and is also the most frequent cause of treatment discontinuation in these trials. If hematocrit rises above 54%, testosterone therapy should be stopped until hematocrit has fallen to <50%. After evaluation of the patient for hypoxia and sleep apnea, testosterone therapy may be reinitiated at a lower dose. However, androgen administration can exacerbate preexisting metastatic prostate cancer. It is not known whether long-term testosterone administration will induce these microscopic foci to grow into clinically significant cancers. Adjust the number of pellets and/or the dosing interval to achieve serum testosterone levels in the normal range. If hematocrit is >54%, stop therapy until hematocrit decreases to a safe level; evaluate the patient for hypoxia and sleep apnea; reinitiate therapy with a reduced dose. Evaluate formulation-specific adverse effects at each visit: uccaltestosteronetablets*: Inquire about alterations in taste and B examine the gums and oral mucosa for irritation. Source: Reproduced with permission from the Endocrine Society Guideline for Testosterone Therapy of Androgen Deficiency Syndromes in Adult Men (Bhasin S et al: J Clin Endocrinol Metab 95:2536, 2010). Cardiovascular Risk As discussed above, there is insufficient evidence to determine whether testosterone replacement therapy increases the risk of major adverse cardiovascular events in hypogonadal men. A large prospective randomized trial is being planned to determine the effects of testosterone replacement therapy on major adverse cardiovascular events in middle-aged and older men with low testosterone levels and symptoms of androgen deficiency. The causes of death among power lifters included suicides, myocardial infarction, and hepatic coma. Orally administered androgens also have been associated with insulin resistance and diabetes. However, if needed, accredited laboratories use gas chromatography-mass spectrometry or liquid chromatography-mass spectrometry to detect anabolic steroid abuse. In recent years, the availability of high-resolution mass spectrometry and tandem mass spectrometry has further improved the sensitivity of detecting androgen abuse. Ratios above 4 suggest exogenous testosterone use but can also reflect genetic variation. Synthetic testosterone has a lower 13C:12C ratio than endogenously produced testosterone and these differences in 13C:12C ratio can be detected by isotope ratio combustion mass spectrometry, which is used to confirm exogenous testosterone use in individuals with a high testosterone to epitestosterone ratio. Basaria S et al: Effects of testosterone administration for 3 years on subclinical atherosclerosis progression in older men with low or low-normal testosterone levels: A randomized clinical trial. Bhasin S et al: Testosterone therapy in men with androgen deficiency syndromes: An endocrine society clinical practice guideline. Bhasin S et al: Effect of testosterone supplementation with and without a dual 5-reductase inhibitor on fat-free mass in men with suppressed testosterone production: a randomized controlled trial. Hall the female reproductive system regulates the hormonal changes responsible for puberty and adult reproductive function. Normal reproductive function in women requires the dynamic integration of hormonal signals from the hypothalamus, pituitary, and ovary, resulting in repetitive cycles of follicle development, ovulation, and preparation of the endometrial lining of the uterus for implantation should conception occur. It is critical to understand pubertal development in normal girls (and boys) as a yardstick for identifying precocious and delayed puberty. To achieve these functions in repeated monthly cycles, the ovary undergoes some of the most dynamic changes of any organ in the body. Primordial germ cells can be identified by the third week of gestation, and their migration to the genital ridge is complete by 6 weeks of gestation. Germ cells persist within the genital ridge, are then referred to as oogonia, and are essential for induction of ovarian development. In patients with 45,X Turner syndrome, primordial germ cells proliferate and migrate to the genital ridge, but do not persist as their survival requires the presence of pregranulosa cells that are dependent on the presence of both X chromosomes. The germ cell population expands, and starting at ~8 weeks of gestation, oogonia begin to enter prophase of the first meiotic division and become primary oocytes. Granulosa cells are derived from mesonephric cells that invade the ovary early in its development, pushing the germ cells to the periphery. Although there is evidence that both oocyte-like cells and follicle-like structures can form from embryonic stem cells in culture, there is, as yet, no clear evidence that this occurs in vivo and thus, the ovary appears to contain a nonrenewable pool of germ cells. It appears that entry into meiosis provides some degree of protection from programmed cell death. The oocyte persists in prophase of the first meiotic division until just before ovulation, when meiosis resumes. The quiescent primordial follicles are recruited to further growth and differentiation through a highly regulated process that limits the size of the developing cohort to ensure that folliculogenesis can continue throughout the reproductive life span. The theca interna cells that surround the developing follicle begin to form as the primary follicle grows. Acquisition of a zona pellucida by the oocyte and the presence of several layers of surrounding cuboidal granulosa cells mark the development of secondary follicles. Bidirectional signaling between the germ cells and the somatic cells in the ovary is a necessary component underlying the maturation of the oocyte and the capacity for hormone secretion. The early stages of follicle growth are primarily driven by intraovarian factors; after initial recruitment, development to the secondary follicle stage may take close to a year. They migrate along the scaffold of the olfactory neurons across the cribiform plate to the hypothalamus where they separate from the olfactory neurons. Thus, like the ovary, the hypothalamic and pituitary components of the reproductive system are present before birth. However, the high levels of estradiol and progesterone produced by the placenta suppress hypothalamic-pituitary stimulation of ovarian hormonal secretion in the fetus. Ovulation requires production of extracellular matrix leading to expansion of the cumulus cell population that surrounds the oocyte and the controlled expulsion of the egg and follicular fluid. Both progesterone and prostaglandins (induced by the ovulatory stimulus) are essential for this process as are members of the matrix metalloproteinase family. Gonadotropin levels are cyclic during the reproductive years and increase dramatically with the loss of negative feedback that accompanies menopause. Metabolic signals, including adipocyte-derived leptin, play a permissive role in reproductive function (Chap. The sequence of steps and the enzymes involved in the synthesis of steroid hormones are similar in the ovary, adrenal, and testis. However, the enzymes required to catalyze specific steps are compartmentalized and may not be abundant or even present in all cell types. These steroid precursors cross the basal lamina to the granulosa cells, which receive no direct blood supply. The hilar interstitial cells of the ovary are functionally similar to Leydig cells and are also capable of secreting androgens. However, high levels of androgens may be produced by luteinized theca cells in women with hyperthecosis. As in the follicle, both cell types are required for steroidogenesis in the corpus luteum. The luteinized granulosa cells are the main source of progesterone production, whereas the smaller theca lutein cells produce 17-hydroxyprogesterone and androgenic substrates for aromatization to estradiol by the luteinized granulosa cells. Production of estrogen metabolites by the corpus luteum plays a significant role in maintenance of the vascularization required for its function. Steroid Hormone Actions Both estrogen and progesterone play critical roles in the expression of secondary sexual characteristics in women (Chap. Estrogen promotes development of the ductule system in the breast, whereas progesterone is responsible for glandular development. In the reproductive tract, estrogens create a receptive environment for fertilization and support pregnancy and parturition through carefully coordinated changes in the endometrium, thickening of the vaginal mucosa, thinning of the cervical mucus, and uterine growth and contractions. Progesterone induces secretory activity in the estrogen-primed endometrium, increases the viscosity of cervical mucus, and inhibits uterine contractions. Both gonadal steroids play critical roles in negative and positive feedback of gonadotropin secretion. Progesterone also increases basal body temperature and has therefore been used clinically as a marker of ovulation. The vast majority of circulating estrogens and androgens are carried in the blood bound to carrier proteins, which restrain their free diffusion into cells and prolong their clearance, serving as a reservoir. Inhibin A is present in both granulosa and theca cells and is secreted by the dominant follicle. Inhibin A is also present in luteinized granulosa cells and is a major secretory product of the corpus luteum. Inhibins function as potent antagonists of activins through sequestration of the activin receptors. For the majority of the cycle, the reproductive system functions in a classic endocrine negative feedback mode. The resultant granulosa cell proliferation is responsible for increasing early follicular phase levels of inhibin B. Increasing levels of estradiol are responsible for proliferative changes in the endometrium. Luteal phase length is relatively constant between 12 and 14 days in normal cycles; thus, the major variability in cycle length is due to variations in follicular phase length. The duration of menstrual bleeding in ovulatory cycles varies between 4 and 6 days. There is a gradual shortening of cycle length with age such that women aged >35 years have cycles that are shorter than during their younger reproductive years. Anovulatory cycles increase as women approach menopause, and bleeding patterns may be erratic. Women who report regular monthly bleeding with cycles that do not vary by >4 days generally have ovulatory cycles, but several other clinical signs can be used to assess the likelihood of ovulation. Some women experience mittelschmerz, described as midcycle pelvic discomfort that is thought to be caused by the rapid expansion of the dominant follicle at the time of ovulation. A constellation of premenstrual moliminal symptoms such as bloating, breast tenderness, and food cravings often occur several days before menses in ovulatory cycles, but their absence cannot be used as evidence of anovulation. Methods that can be used to determine whether ovulation is likely include a serum progesterone level >5 ng/mL ~7 days before expected menses, an increase in basal body temperature of 0. Ultrasound can be used to detect the growth of the fluid-filled antrum of the developing follicle and to assess endometrial proliferation in response to increasing estradiol levels in the follicular phase. It can also be used to provide evidence of ovulation by documenting collapse of the dominant follicle and/or the presence of a corpus luteum as well as the characteristic echogenicity of the secretory endometrium of the luteal phase. The triggers for adrenarche remain unknown but may involve increases in body mass index, as well as in utero and neonatal factors. The breast is exquisitely sensitive to the very low levels of estrogen that result from peripheral conversion of adrenal androgens and the low levels of estrogen secreted from the ovary early in pubertal maturation. Breast development precedes the appearance of pubic and axillary hair in ~60% of girls. There has been a gradual decline in the age of menarche over the past century, attributed in large part to improvement in nutrition, and there is a relationship between adiposity and earlier sexual maturation in girls. Progesterone and inhibin A are produced from the luteinized granulosa cells, which continue to aromatize theca-derived androgen precursors, producing estradiol. The combined actions of estrogen and progesterone are responsible for the secretory changes in the endometrium that are necessary for implantation.
Diets containing low-energy-dense foods have been shown to control hunger and thus to result in decreased caloric intake and weight loss gastritis video best buy nexium. These conditions include poorly controlled type 2 diabetes gastritis diet 321 generic nexium 20 mg online, hypertriglyceridemia gastritis untreated nexium 20mg cheap, obstructive sleep apnea gastritis diet vs exercise purchase nexium 40mg visa, and symptomatic peripheral edema gastritis diet ��������� discount 20 mg nexium with visa. This algorithm applies to the assessment of overweight and obesity and subsequent decisions based on that assessment gastritis diet ���� best order for nexium. Prophylaxis against gallstone formation with ursodeoxycholic acid (600 mg/d) is effective in reducing this risk. Medical supervision is required because of the rapid rate of weight loss and potential for health complications. Physical Activity Therapy Although exercise alone is only moderately effective for weight loss, the combination of dietary modification and exercise is the most effective behavioral approach for the treatment of obesity. The most important role of exercise appears to be in the maintenance of the weight loss. Focusing on simple ways to add physical activity into the normal daily routine through leisure activities, travel, and domestic work should be suggested. Examples include brisk walking, using the stairs, doing housework and yard work, and engaging in sports. Asking the patient to wear a pedometer or accelerometer to monitor total accumulation of steps or kcal expended as part of the activities of daily living is a useful strategy. Studies have demonstrated that lifestyle activities are as effective as structured exercise programs for improving cardiorespiratory fitness and weight loss. A high level of physical activity (>300 min of moderate-intensity activity per week) is often needed to lose weight and sustain weight loss. These exercise recommendations are daunting to most patients and need to be implemented gradually. Behavioral Therapy Cognitive behavioral therapy is used to help change and reinforce new dietary and physical activity behaviors. When recommending any behavioral lifestyle change, the patient should be asked to identify what, when, where, and how the behavioral change will be performed. The patient should keep a record of the anticipated behavioral change so that progress can be reviewed at the next office visit. Because these techniques are time consuming to implement, their supervision is often undertaken by ancillary office staff, such as a nurse-clinician or registered dietitian. When an antiobesity medication is prescribed, patients should be actively engaged in a lifestyle program that provides the strategies and skills needed to use the drug effectively, since such support increases total weight loss. Medications for obesity have traditionally fallen into two major categories: appetite suppressants (anorexiants) and gastrointestinal fat blockers. Gastrointestinal fat blockers reduce the absorption of selective macronutrients, such as fat, from the gastrointestinal tract. Centrally Acting Anorexiant Medications Anorexiants affect satiety (the absence of hunger after eating) and hunger (the biologic sensation that prompts eating). By increasing satiety and decreasing hunger, these agents help patients reduce caloric intake without a sense of deprivation. The target site for the actions of anorexiants is the ventromedial and lateral hypothalamic regions in the central nervous system (Chap. The classic sympathomimetic adrenergic agents (benzphetamine, phendimetrazine, diethylpropion, mazindol, and phentermine) function by stimulating norepinephrine release or by blocking its reuptake. Among the anorexiants, phentermine is the most commonly prescribed; there are limited long-term data on its effectiveness. A 2002 review of six randomized, placebo-controlled trials of phentermine for weight control found that patients lost 0. The most common side effects of the amphetamine-derived anorexiants are restlessness, insomnia, dry mouth, constipation, and increased blood pressure and heart rate. Weight loss was identified as an unintended side effect of topiramate during clinical trials for epilepsy. Clinical and statistical dose-dependent improvements were seen in selected cardiovascular and metabolic outcome measurements that were related to the weight loss. The most common adverse events experienced by the drug-randomized group were paresthesias, dry mouth, constipation, dysgeusia, and insomnia. Because of an increased risk of congenital fetal oral-cleft formation from topiramate, women of childbearing age should have a negative pregnancy test before treatment and monthly thereafter, and use effective contraception consistently during medication therapy. Lorcaserin has undergone two randomized, placebo-controlled, double-blind trials for efficacy and safety. Participant numbers, eligibility, characteristics, and weight-loss outcomes are displayed in Table 395-5. Patients who were overweight or obese had at least one coexisting condition (hypertension, dyslipidemia, cardiovascular disease, impaired glucose tolerance, or sleep apnea)-medical conditions that are commonly seen in the office setting. Modest statistical improvements consistent with the weight loss were seen in selected cardiovascular and metabolic outcome measurements. The most common adverse events experienced by the drug group were headache, dizziness, and nausea. The medication has undergone three randomized, placebocontrolled, double-blind trials for efficacy and safety. However, the medication led to slight increased or smaller decreases in blood pressure and pulse than placebo. The most common adverse events experienced by the drug-randomized groups were nausea, constipation, headache, vomiting, dizziness, diarrhea, insomnia, and dry mouth. Liraglutide has undergone three randomized, placebo-controlled, double-blind trials for efficacy and safety. Clinical and statistical dose-dependent improvements were seen in selected cardiovascular and metabolic outcome measurements; however, there is a small increase in heart rate. The most common adverse effects include nausea, diarrhea, constipation, and vomiting. Determining responsiveness at 3 or 4 months is based on the post hoc observed trial data that patients who did not lose a prespecified amount of weight early in treatment were less successful at 1 year. This drug is a potent, slowly reversible inhibitor of pancreatic, gastric, and carboxylester lipases and phospholipase A2, which are required for the hydrolysis of dietary fat into fatty acids and monoacylglycerols. Orlistat acts in the lumen of the stomach and small intestine by forming a covalent bond with the active site of these lipases. Taken at a therapeutic dose of 120 mg tid, orlistat blocks the digestion and absorption of ~30% of dietary fat. Because orlistat is minimally (<1%) absorbed from the gastrointestinal tract, it has no systemic side effects. Adverse gastrointestinal effects, including flatus with discharge, fecal urgency, fatty/oily stool, and increased defecation, are reported in at least 10% of orlistat-treated patients. These side effects generally are experienced early, diminish as patients control their dietary fat intake, and only infrequently cause patients to withdraw from clinical trials. When taken concomitantly, psyllium mucilloid is helpful in controlling orlistat-induced gastrointestinal side effects. Because serum concentrations of the fat-soluble vitamins D and E and -carotene may be reduced by orlistat treatment, vitamin supplements are recommended to prevent potential deficiencies. Weight-loss surgeries have traditionally been classified into three categories on the basis of anatomic changes: restrictive, restrictive malabsorptive, and malabsorptive. More recently, however, the clinical benefits of bariatric surgery in achieving weight loss and alleviating metabolic comorbidities have been attributed largely to changes in the physiologic responses of gut hormones, bile acid metabolism, the microbiota, and in adipose tissue metabolism. Additional effects on food intake and body weight control may be attributed to changes in vagal signaling. The loss of fat mass, particularly visceral fat, is associated with multiple metabolic, adipokine, and inflammatory changes that include improved insulin sensitivity and glucose disposal; reduced free fatty acid flux; increased adiponectin levels; and decreased interleukin 6, tumor necrosis factor, and high-sensitivity C-reactive protein levels. Restrictive surgeries limit the amount of food the stomach can hold and slow the rate of gastric emptying. In contrast to previous devices, these bands have diameters that are adjustable by way of their connection to a reservoir that is implanted under the skin. In the laparoscopic sleeve gastrectomy, the stomach is restricted by stapling and dividing it vertically, removing ~80% of the greater curvature and leaving a slim banana-shaped remnant stomach along the lesser curvature. Weight loss after this procedure is superior to that after laparoscopic adjustable gastric banding. Examples of operative interventions used for surgical manipulation of the gastrointestinal tract. Significant improvement in multiple obesity-related comorbid conditions, including type 2 diabetes, hypertension, dyslipidemia, obstructive sleep apnea, quality of life, and long-term cardiovascular events, has been reported. Among the observed improvements in comorbidities, the prevention and treatment of type 2 diabetes resulting from bariatric surgery has garnered the most attention. Fifteen-year data from the Swedish Obese Subjects study demonstrated a marked reduction. Several randomized controlled studies have shown greater weight loss and more improved glycemic control at 1 and 3 years among surgical patients than among patients receiving conventional medical therapy. However, among these patients, one-third redeveloped type 2 diabetes within 5 years. The rapid improvement seen in diabetes after restrictive-malabsorptive procedures is thought to be due to caloric restriction, reduced insulin resistance, and surgery-specific effects on glucose homeostasis brought about by alteration of gut hormones. These complications typically are treated by endoscopic balloon dilation and acid suppression therapy, respectively. For patients who undergo laparoscopic adjustable gastric banding, there are no intestinal absorptive abnormalities other than mechanical reduction in gastric size and outflow. Therefore, selective deficiencies are uncommon unless eating habits become unbalanced. In contrast, the restrictive-malabsorptive procedures carry an increased risk for micronutrient deficiencies of vitamin B12, iron, folate, calcium, and vitamin D. Patients with restrictive-malabsorptive procedures require lifelong supplementation with these micronutrients. However, there is increasing recognition of other forms of diabetes in which the molecular pathogenesis is better understood and may be associated with a single gene defect. Arrows indicate that changes in glucose tolerance may be bidirectional in some types of diabetes. Genetic defects of beta cell development or function characterized by mutations in: 1. Genetic defects in insulin action, including type A insulin resistance, Leprechaunism, Rabson-Mendenhall syndrome, Lipodystrophy syndromes E. Uncommon forms of immune-mediated diabetes-"stiff-person" syndrome, anti-insulin receptor antibodies I. Mutations in the insulin receptor cause a group of rare disorders characterized by severe insulin resistance. A form of acute onset of type 1 diabetes, termed fulminant diabetes, has been noted in Japan and may be related to viral infection of the islets. Both type 1 and type 2 diabetes are preceded by a period of progressive worsening of glucose homeostasis, followed by the development of hyperglycemia that exceeds the threshold for clinical diagnosis. The countries with the greatest number of individuals with diabetes in 2015 are China (109. Approximately 25% of the individuals with diabetes in the United States were undiagnosed; globally, it is estimated that as many of 50% of individuals with diabetes may be undiagnosed. Global estimate is 415 million individuals with diabetes mia at which diabetes-specific complications occur rather than deviation from in 2017. For example, the prevalence of retinopathy in Native the United Sates was estimated to be 0. Northern Europe and the United same individuals, but individuals in all three groups are at greater risk States have an intermediate rate. Some use the terms prediabetes, increased risk of diabetes, or intermediate hyperglycemia (World Health Organization) and slightly locations. However, now populations less enriched with these classic high-risk different metrics for this category. However, some 2012) was 8% in non-Hispanic whites, 9% in Asian Americans, 13% in individuals may meet criteria for one test but not the other. Also, it is Hispanics, 13% in non-Hispanic blacks, and 16% in American-Indian and important to note that race and ethnicity may impact the reliability of Alaskan native populations. For example, African Americans have a higher HbA1c at an earlier age in ethnic groups other than non-Hispanic whites. In 2015, it was estimated be performed in aStandardization Program and correlated to the reference assay Glycohemoglobin that $673 billion or 12% of health care expenditures worldwide were of the Diabetes Control and Complications Trial.
Purchase generic nexium. HCG Diet and HCG Side Effects on Action 3 News -- Lose Weight FAST.
With current therapies gastritis diet ���� generic nexium 20 mg visa, affected individuals can survive into the late forties with satisfactory quality of life diet gastritis kronik nexium 20mg with visa. The first clues to defining the anatomic area of involvement appear in the history gastritis diet xtreme generic nexium 40mg fast delivery, and the examination is then directed to confirm or rule out these impressions and to clarify uncertainties gastritis meals best order for nexium. For example gastritis onions buy nexium 40 mg with visa, the examination of a patient who presents with a history of ascending paresthesias and weakness should be directed toward deciding gastritis diet x program nexium 40mg online, among other things, if the lesion is in the spinal cord or peripheral nerves. Focal back pain, a spinal cord sensory level, and incontinence suggest a spinal cord origin, whereas a stocking-glove pattern of sensory loss suggests peripheral nerve disease; areflexia usually indicates peripheral neuropathy but may also be present with spinal shock in acute spinal cord disorders. Deciding "where the lesion is" accomplishes the task of limiting the possible etiologies to a manageable, finite number. Symptoms of recurrent vertigo, diplopia, and nystagmus should not trigger "multiple sclerosis" as an answer (etiology) but "brainstem" or "pons" (location); then a diagnosis of brainstem arteriovenous malformation will not be missed for lack of consideration. Clues to the pathophysiology of the disease process may also be present in the history. Primary neuronal (gray matter) disorders often present as early cognitive disturbances, movement disorders, or seizures, whereas white matter involvement produces "long tract" disorders of motor, sensory, visual, and cerebellar pathways. Progressive and symmetric symptoms often have a metabolic or degenerative origin; in such cases lesions are usually not sharply circumscribed. Thus, a patient with paraparesis and a clear spinal cord sensory level is unlikely to have vitamin B12 deficiency as the explanation. A patient with recurrent episodes of diplopia and dysarthria associated with exercise or fatigue may have a disorder of neuromuscular transmission such as myasthenia gravis. Slowly advancing visual scotoma with luminous edges, termed fortification spectra, indicates spreading cortical depression, typically with migraine. According to estimates by the World Health Organization, neurologic disorders affect over 1 billion people worldwide, constitute 12% of the global burden of disease, and cause 14% of global deaths (Table 415-1). Because therapies now exist for many neurologic disorders, a skillful approach to diagnosis is essential. Errors commonly result from an overreliance on costly neuroimaging procedures and laboratory tests, which, while useful, do not substitute for an adequate history and examination. The proper approach begins with the patient and focuses the clinical problem first in anatomic and then in pathophysiologic terms; only then should a specific neurologic diagnosis be entertained. This method ensures that technology is judiciously applied, a correct diagnosis is established in an efficient manner, and treatment is promptly initiated. Can the disorder be mapped to one specific location, is it multifocal, or is a diffuse process present Are the symptoms restricted to the nervous system, or do they arise in the context of a systemic illness Attention to the description of the symptoms experienced by the patient and substantiated by family members and others often permits an accurate localization and determination of the probable cause, even before the neurologic examination is performed. Each complaint should be pursued as far as possible to identify the location of the lesion, the likely underlying pathophysiology, and potential etiologies. Does the patient have difficulty with brushing hair or reaching upward (proximal) or buttoning buttons or opening a twist-top bottle (distal) A patient with a right hemiparesis without a language deficit likely has a lesion (internal capsule, brainstem, or spinal cord) different from that of a patient with a right hemiparesis and aphasia (left hemisphere). The rapid onset of a neurologic complaint, occurring within seconds or minutes, usually indicates a vascular event, a seizure, or migraine. The onset of sensory symptoms located in one extremity that spread over a few seconds to adjacent portions of that extremity and then to the other regions of the body suggests a seizure. A similar but slower temporal march of symptoms accompanied by headache, nausea, or visual disturbance suggests migraine. A stuttering onset where symptoms appear, stabilize, and then progress over hours or days also suggests cerebrovascular disease; an additional history of transient remission or regression indicates that the process is more likely due to ischemia rather than hemorrhage. A gradual evolution of symptoms over hours or days suggests a toxic, metabolic, infectious, or inflammatory process. Progressing symptoms associated with the systemic manifestations of fever, stiff neck, and altered level of consciousness imply an infectious process. Slowly progressive symptoms without remissions are characteristic of neurodegenerative disorders, chronic infections, gradual intoxications, and neoplasms. The interpretation of the true meaning of the words used by patients to describe symptoms obviously becomes even more complex when there are differences in primary languages and cultures. Episodes of loss of consciousness necessitate that details be sought from observers to ascertain precisely what has happened during the event. It is important to elicit family history about all illnesses, in addition to neurologic and psychiatric disorders. A familial propensity to hypertension or heart disease is relevant in a patient who presents with a stroke. There are numerous inherited neurologic diseases that are associated with multisystem manifestations that may provide clues to the correct diagnosis. Diabetes mellitus, hypertension, and abnormalities of blood lipids predispose to cerebrovascular disease. Patients with malignancy may also present with a neurologic paraneoplastic syndrome (Chap. Various neurologic disorders occur with dysthyroid states or other endocrinopathies. It is especially important to look for the presence of systemic diseases in patients with peripheral neuropathy. Most patients with coma in a hospital setting have a metabolic, toxic, or infectious cause. It is essential to inquire about the history of drug use, both prescribed and illicit. Sedatives, antidepressants, and other psychoactive medications are frequently associated with acute confusional states, especially in the elderly. Aminoglycoside antibiotics may exacerbate symptoms of weakness in patients with disorders of neuromuscular transmission, such as myasthenia gravis, and may cause dizziness secondary to ototoxicity. Vincristine and other antineoplastic drugs can cause peripheral neuropathy, and immunosuppressive agents such as cyclosporine can produce encephalopathy. Excessive vitamin ingestion can lead to disease; examples include vitamin A and pseudotumor cerebri or pyridoxine and peripheral neuropathy. Many patients are unaware that over-the-counter sleeping pills, cold preparations, and diet pills are actually drugs. Alcohol, the most prevalent neurotoxin, is often not recognized as such by patients, and other drugs of abuse such as cocaine and heroin can cause a wide range of neurologic abnormalities. Use the opportunity while taking the history to form an impression of the patient. Are there any clues to problems with language, memory, insight, comportment, or behavior The neurologic assessment begins as soon as the patient comes into the room and the first introduction is made. Mastery of the complete neurologic examination is usually important only for physicians in neurology and associated specialties. However, knowledge of the basics of the examination, especially those components that are effective in screening for neurologic dysfunction, is essential for all clinicians, especially generalists. Whether the examination is basic or comprehensive, it is essential that it is performed in an orderly and systematic fashion to avoid errors and serious omissions. The detailed description that follows describes the more commonly used parts of the neurologic examination, with a particular emphasis on the components that are considered most helpful for the assessment of common neurologic problems. Each section also includes a brief description of the minimal examination necessary to adequately screen for abnormalities in a patient who has no symptoms suggesting neurologic dysfunction. First, in recording observations, it is important to describe what is found rather than to apply a poorly defined medical term. If the complaint is of dizziness when the head is turned in one direction, have the patient do this and also look for associated signs on examination. If pain occurs after walking two blocks, have the patient leave the office and walk this distance and immediately return, and repeat the relevant parts of the examination. The mental status examination is under way as soon as the physician begins observing and speaking with the patient. If the history raises any concern for abnormalities of higher cortical function or if cognitive problems are observed during the interview, then detailed testing of the mental status is indicated. Using ageadjusted values for defining normal performance, the test is ~85% sensitive and 85% specific for making the diagnosis of dementia that is moderate or severe, especially in educated patients. Individual elements of the mental status examination can be subdivided into level of consciousness, orientation, speech and language, memory, fund of information, insight and judgment, abstract thought, and calculations. When the patient is not fully awake, the examiner should describe the responses to the minimum stimulus necessary to elicit a reaction, ranging from verbal commands to a brief, painful stimulus such as a squeeze of the trapezius muscle. Responses that are directed toward the stimulus and signify some degree of intact cerebral function. Orientation is tested by asking the person to state his or her name, location, and time (day of the week and date); time is usually the first to be affected in a variety of conditions. A typical testing sequence is to ask the patient to name successively more detailed components of clothing, a watch, or a pen; repeat the phrase "No ifs, ands, or buts"; follow a three-step, verbal command; write a sentence; and read and respond to a written command. Memory should be analyzed according to three main time scales: (1) immediate memory is assessed by saying a list of three items and having the patient repeat the list immediately; (2) short-term memory is tested by asking the patient to recall the same three items 5 and 15 min later; and (3) long-term memory is evaluated by determining 3027 how well the patient is able to provide a coherent chronologic history of his or her illness or personal events. Fund of information is assessed by asking questions about major historic or current events, with special attention to educational level and life experiences. Abnormalities of insight and judgment are usually detected during the patient interview; a more detailed assessment can be elicited by asking the patient to describe how he or she would respond to situations having a variety of potential outcomes. Abstract thought can be tested by asking the patient to describe similarities between various objects or concepts. With eyes closed, ask the patient to sniff a mild stimulus such as toothpaste or coffee and identify the odorant. As a screening test, it is usually sufficient to examine the visual fields of both eyes simultaneously; individual eye fields should be tested if there is any reason to suspect a problem of vision by the history or other elements of the examination, or if the screening test reveals an abnormality. Instruct the patient to look directly at the center of your face and to indicate when and where he or she sees one of your fingers moving. Beginning with the two inferior quadrants and then the two superior quadrants, move your index finger of the right hand, left hand, or both hands simultaneously and observe whether the patient detects the movements. A single small-amplitude movement of the finger is sufficient for a normal response. Focal perimetry and tangent screen examinations should be used to map out visual field defects fully or to search for subtle abnormalities. Optic fundi should be examined with an ophthalmoscope, and the color, size, and degree of swelling or elevation of the optic disc noted, as well as the color and texture of the retina. The retinal vessels should be checked for size, regularity, arteriovenous nicking at crossing points, hemorrhage, exudates, etc. To check extraocular movements, ask the patient to keep his or her head still while tracking the movement of the tip of your finger. Move the target slowly in the horizontal and vertical planes; observe any paresis, nystagmus, or abnormalities of smooth pursuit (saccades, oculomotor ataxia, etc. If necessary, the relative position of the two eyes, both in primary and multidirectional gaze, can be assessed by comparing the reflections of a bright light off both pupils. However, in practice it is typically more useful to determine whether the patient describes diplopia in any direction of gaze; true diplopia should almost always resolve with one eye closed. As with other parts of the sensory examination, testing of two sensory modalities derived from different anatomic pathways. Look in particular for differences in the lower versus upper facial muscles; weakness of the lower twothirds of the face with preservation of the upper third suggests an upper motor neuron lesion, whereas weakness of an entire side suggests a lower motor neuron lesion. Increased tone may be evident as spasticity (resistance determined by the angle and velocity of motion; corticospinal tract disease), rigidity (similar resistance in all angles of motion; extrapyramidal disease), or paratonia (fluctuating changes in resistance; frontal lobe pathways or normal difficulty in relaxing). Cogwheel rigidity, in which passive motion elicits jerky interruptions in resistance, is seen in parkinsonism. Strength Testing for pronator drift is an extremely useful method hear a finger rub or whispered voice with each ear. Further testing for air versus mastoid bone conduction (Rinne) and lateralization of a 512-Hz tuning fork placed at the center of the forehead (Weber) should be done if an abnormality is detected by history or examination. For further discussion of assessing vestibular nerve function in the setting of dizziness, hearing loss, or coma, see Chaps. The patient is asked to hold both arms fully extended and parallel to the ground with eyes closed. This position should be maintained for ~10 s; any flexion at the elbow or fingers or pronation of the forearm, especially if asymmetric, is a sign of potential weakness. Muscle strength is further assessed by having the patient exert maximal effort for the particular muscle or muscle group being tested. The pharyngeal ("gag") reflex is evaluated by stimulating the posterior pharyngeal wall on each side with a sterile, blunt object. However, in many cases, it is more practical to use the following terms: Paralysis = no movement Severe weakness = movement with gravity eliminated Moderate weakness = movement against gravity but not against mild resistance Mild weakness = movement against moderate resistance Full strength Noting the pattern of weakness is as important as assessing the magnitude of weakness. Unilateral or bilateral weakness of the upper limb extensors and lower limb flexors ("pyramidal weakness") suggests a lesion of the pyramidal tract, bilateral proximal weakness suggests myopathy, and bilateral distal weakness suggests peripheral neuropathy. Assess upper extremity strength by checking for pronator drift and strength of wrist or finger extensors. Assess lower extremity strength by checking strength of the toe extensors and having the patient walk normally and on heels and toes. The motor examination includes observations of muscle appearance, tone, and strength. Although gait is in part a test of motor function, it is usually evaluated separately at the end of the examination.
However atrophic gastritis symptoms uk cheap nexium 40mg fast delivery, ultrasound is not indicated if the thyroid physical examination is normal gastritis diet therapy order nexium pills in toronto. A bruit or thrill over the gland gastritis symptoms nhs nexium 20mg low cost, located over the insertion of the superior and inferior thyroid arteries (supero- or inferolaterally) gastritis or ulcer order nexium 40mg with amex, indicates increased vascularity gastritis diet 2013 cheap nexium 20mg fast delivery, associated with turbulent rather than laminar blood flow gastritis diet 500 discount nexium 40 mg, as occurs in hyperthyroidism. If the lower borders of the thyroid lobes are not clearly felt, a goiter may be retrosternal. With any central mass above the thyroid, the tongue should be extended, as thyroglossal cysts then move upward. The thyroid examination is not complete without assessment for lymphadenopathy in the supraclavicular and cervical regions of the neck. T4 and T3 are highly protein-bound, and numerous factors (illness, medications, genetic factors) can influence protein binding. It is useful, therefore, to measure the free, or unbound, hormone levels, which correspond to the biologically available hormone pool. Two direct methods are used to measure unbound thyroid hormones: (1) unbound thyroid hormone competition with radiolabeled T4 (or an analogue) for binding to a solid-phase antibody, and (2) physical separation of the unbound hormone fraction by ultracentrifugation or equilibrium dialysis. Although early unbound hormone immunoassays suffered from artifacts, newer assays correlate well with the results of the more technically demanding and expensive physical separation methods. The latter is derived from the T3-resin uptake test, which determines the distribution of radiolabeled T3 between an absorbent resin and the unoccupied thyroid hormone binding proteins in the sample. The binding of the labeled T3 to the resin is increased when there is reduced unoccupied protein binding sites. In effect, the index corrects for anomalous total hormone values caused by variations in hormone-protein binding. Because unbound thyroid hormone levels are normal and the patient is euthyroid in all of these circumstances, assays that measure unbound hormone are preferable to those for total thyroid hormones. Tests for the end-organ effects of thyroid hormone excess or depletion, such as estimation of basal metabolic rate, tendon reflex relaxation rates, or serum cholesterol, are relatively insensitive and are not useful as clinical determinants of thyroid function. Serum Tg levels are increased in all types of thyrotoxicosis except thyrotoxicosis factitia caused by self-administration of thyroid hormone. Tg levels are particularly increased in thyroiditis, reflecting thyroid tissue destruction and release of Tg. The main role for Tg measurement, however, is in the follow-up of thyroid cancer patients. After total 2698 thyroidectomy and radioablation, Tg levels should be undetectable; in the absence of anti-Tg antibodies, measurable levels indicate incomplete ablation or recurrent cancer. Radioiodine Uptake and Thyroid Scanning the thyroid gland selectively transports radioisotopes of iodine (123I, 125I, 131I) and 99m Tc pertechnetate, allowing thyroid imaging and quantitation of radioactive tracer fractional uptake. Toxic adenomas appear as focal areas of increased uptake, with suppressed tracer uptake in the remainder of the gland. Whole-body and thyroid scanning is also used in the treatment and surveillance of thyroid cancer. Thyroid Ultrasound Ultrasonography is valuable for the diagnosis and evaluation of patients with nodular thyroid disease (Chap. Evidence-based guidelines recommend thyroid ultrasonography for all patients suspected of having thyroid nodules by either physical examination or another imaging study. Sonographic patterns that combine suspicious sonographic features are highly suggestive of malignancy. In addition to evaluating thyroid nodules, ultrasound is useful for monitoring nodule size and for the aspiration of nodules or cystic lesions. Ultrasonography of the central and lateral cervical lymph node compartments is indispensable in the evaluation thyroid cancer patients, preoperatively and during follow-up. In addition, the American College of Radiology recommends a survey of the cervical lymph nodes as part of every diagnostic thyroid sonographic examination. Mutations that cause congenital hypothyroidism are being increasingly identified, but most remain idiopathic (Table 376-2). Transplacental passage of maternal thyroid hormone occurs before the fetal thyroid gland begins to function and provides partial hormone support to a fetus with congenital hypothyroidism. Although some patients may have minor symptoms, this state is called subclinical hypothyroidism. Prevalence the mean annual incidence rate of autoimmune hypo- thyroidism is up to 4 per 1000 women and 1 per 1000 men. It is more common in certain populations, such as the Japanese, probably because of genetic factors and chronic exposure to a high-iodine diet. The mean age at diagnosis is 60 years, and the prevalence of overt hypothyroidism increases with age. In atrophic thyroiditis, the fibrosis is much more extensive, lymphocyte infiltration is less pronounced, and thyroid follicles are almost completely absent. Other congenital malformations, especially cardiac, are four times more common in congenital hypothyroidism. If transient hypothyroidism is suspected, or the diagnosis is unclear, treatment can be stopped safely after the age of 3 years followed by further evaluation. A high iodine or low selenium intake and decreased exposure to microorganisms in childhood increase the risk of autoimmune hypothyroidism. Smoking cessation transiently increases incidence whereas alcohol intake seems protective. These factors may account for the increase in prevalence over the last two to three decades. The thyroid lymphocytic infiltrate in autoimmune hypothyroidism is composed of activated T cells as well as B cells. Novel anticancer and immunomodulatory treatments, such as tyrosine kinase inhibitors and alemtuzumab, can also induce thyroid autoimmunity via their effects on T cell regulation. Predicting the course of disease in such individuals is difficult, and they require close monitoring of thyroid function. The use of these assays does not generally alter clinical management, although it may be useful to confirm the cause of transient neonatal hypothyroidism. Clinical Manifestations the main clinical features of hypothy- roidism are summarized in Table 376-3. The onset is usually insidious, and the patient may become aware of symptoms only when euthyroidism is restored. The skin is dry, and there is decreased sweating, thinning of the epidermis, and hyperkeratosis of the stratum corneum. Increased dermal glycosaminoglycan content traps water, giving rise to skin thickening without pitting (myxedema). There is pallor, often with a yellow tinge to the skin due to carotene accumulation. Nail growth is retarded, and hair is dry, brittle, difficult to manage, and falls out easily. In addition to diffuse alopecia, there is thinning of the outer third of the eyebrows, although this is not a specific sign of hypothyroidism. Other common features include constipation and weight gain (despite a poor appetite). In contrast to popular perception, the weight gain is usually modest and due mainly to fluid retention in the myxedematous tissues. Libido is decreased in both sexes, and there may be oligomenorrhea or amenorrhea in long-standing disease, but menorrhagia may occur at an early stage. Myocardial contractility and pulse rate are reduced, leading to a reduced stroke volume and bradycardia. Increased peripheral resistance may be accompanied by hypertension, particularly diastolic. Pericardial effusions occur in up to 30% of patients but rarely compromise cardiac function. Although alterations in myosin heavy chain isoform expression have been documented, cardiomyopathy is rare. Fluid may also accumulate in other serous cavities and in the middle ear, giving rise to conductive deafness. Pulmonary function is generally normal, but dyspnea may be caused by pleural effusion, impaired respiratory muscle function, diminished ventilatory drive, or sleep apnea. Carpal tunnel and other entrapment syndromes are common, as is impairment of muscle function with stiffness, cramps, and pain. On examination, there may be slow relaxation of tendon reflexes and pseudomyotonia. Rare neurologic problems include reversible cerebellar ataxia, dementia, psychosis, and myxedema coma. Other causes of hypothyroidism are discussed below and in Table 376-1 but rarely cause diagnostic confusion. Iatrogenic hypothyroidism is a common cause of hypothyroidism and can often be detected by screening before symptoms develop. Low-dose thyroxine treatment hypothyroidism causes of hypothyroidism can be withdrawn if recovery occurs. Iodine deficiency is responsible for endemic goiter and cretinism vocal cords and tongue. The features described above are the consequence of thyroid hor- but is an uncommon cause of adult hypothyroidism unless the iodine mone deficiency. However, autoimmune hypothyroidism may be intake is very low or there are complicating factors, such as the conassociated with signs or symptoms of other autoimmune diseases, par- sumption of thiocyanates in cassava or selenium deficiency. Less common associations include celiac public health measures to improve iodine intake should be advocated disease, dermatitis herpetiformis, chronic active hepatitis, rheumatoid to eliminate this problem. The intracellular events that account for this effect are unclear, but individuals with autoimmune thyroiditis are especially associated with autoimmune hypothyroidism. Iodine excess is responsible for the hypothyroidism that presents with slow growth and delayed facial and dental maturation. Secondary hypothyroidism is usually diagnosed in the context of other In most cases, puberty is delayed, but precocious puberty sometimes occurs. The diagnosis is condetermine the existence and cause of hypothyroidism is provided in firmed by detecting a low unbound T level. In many findings in hypothyroidism may include increased creatine phosphokpatients, however, lower doses suffice until residual thyroid tissue is inase, elevated cholesterol and triglycerides, and anemia (usually nordestroyed. The use of levothyroxine combined with liothyronine (triiodothyronine, T3) has been investigated, but benefit has not been confirmed in prospective studies. There is no place for liothyronine alone as long-term replacement, because the short half-life necessitates three or four daily doses and is associated with fluctuating T3 levels. It is important to ensure ongoing adherence as patients do not feel any symptomatic difference after missing a few doses of levothyroxine, and this sometimes leads to self-discontinuation. Because T4 has a long half-life (7 days), patients who miss a dose can be advised to take two doses of the skipped tablets at once. Other causes of increased levothyroxine requirements must be excluded, particularly malabsorption. Presentation appears to be idiosyncratic and occurs months after treatment has begun. Because maternal hypothyroidism may both adversely affect fetal neural development and be associated with adverse gestational outcomes (miscarriage, preterm delivery), thyroid function should be monitored to preserve euthyroidism in women with a history or high risk of hypothyroidism. The presence of thyroid autoantibodies alone, in a euthyroid patient, is also associated with miscarriage and preterm delivery; large-scale trials are underway to establish whether levothyroxine therapy improves outcomes in this group. Women should increase levothyroxine from once daily dosing to nine doses per week as soon as pregnancy is confirmed, to anticipate this change. Pregnant women should be counseled to separate ingestion of prenatal vitamins and iron supplements from levothyroxine. In the elderly, especially patients with known coronary artery disease, the starting dose of levothyroxine is 12. In some patients, it may be impossible to achieve full replacement despite optimal antianginal treatment. Emergency surgery is generally safe in patients with untreated hypothyroidism, although routine surgery in a hypothyroid patient should be deferred until euthyroidism is achieved. Clinical manifestations include reduced level of consciousness, sometimes associated with seizures, as well as the other features of hypothyroidism (Table 376-3). There may be a history of treated hypothyroidism with poor compliance, or the patient may be previously undiagnosed. Myxedema coma almost always occurs in the elderly and is usually precipitated by factors that impair respiration, such as drugs (especially sedatives, anesthetics, and antidepressants), pneumonia, congestive heart failure, myocardial infarction, gastrointestinal bleeding, or cerebrovascular accidents. Hypoventilation, leading to hypoxia and hypercapnia, plays a major role in pathogenesis; hypoglycemia and dilutional hyponatremia also contribute to the development of myxedema coma. Because T4 T3 conversion is impaired in myxedema coma, there is a rationale for adding liothyronine (T3) intravenously or via nasogastric tube to levothyroxine treatment, although excess liothyronine has the potential to provoke arrhythmias. Supportive therapy should be provided to correct any associated metabolic disturbances.