Amaryl
Aaron E. Chen, MD
- Assistant Professor
- Department of Pediatric Emergency Medicine
- Johns Hopkins University
- Baltimore, Maryland
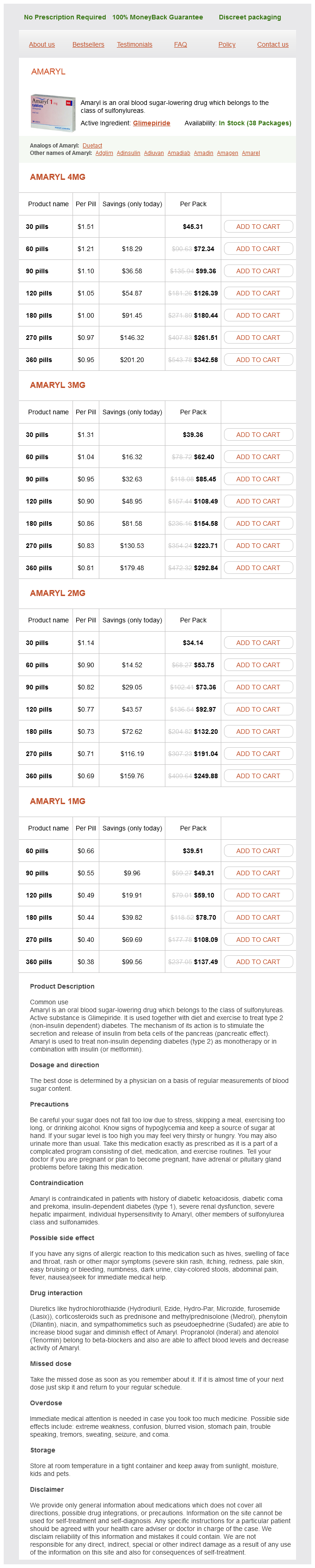
If the degrees of freedom of the relevant t-distribution was not given diabetes control juice order amaryl 2 mg with mastercard, we attempted to back it out of the study based upon the statistical methods that were used as long as we could confidently conclude that it was greater than 25 diabetes symptoms for type 2 purchase amaryl paypal. We also used the Knapp-Hartung adjustment in order to avoid the potentially high inflation of the type-I error rate that can arise when dealing with small numbers of even moderately heterogeneous studies metabolic disease awareness week 2012 buy amaryl pills in toronto. These results are charitably interpreted as providing an estimate of the true average effect among completed trials and are presented along with the results derived from analyses using randomeffect models diabetes medications discounts generic amaryl 4mg with mastercard. Phases were grouped as: (1) acute mania or hypomania metabolic disease you can get from bad purchase cheapest amaryl, including mixed diabetes medicine online shopping buy amaryl 4 mg free shipping, (2) acute depression, (3) any acute state (often for psychosocial maintenance studies), (4) euthymic or subsyndromal (generally for maintenance studies), and (5) nonspecific, that is, either euthymic, acute in any episode, or posthospitalization (these studies stated essentially any patient with bipolar disorder except acute mania). For drug studies treating patients for residual symptoms, patients were classified as nonresponders to standard treatment (usually noted in adjunctive drug studies). Studies were categorized as maintenance studies if the study inclusion criteria did not specify an acute episode at study entry. For acute mania treatment, outcomes were grouped by 3-4 weeks and then final measurement (generally 6 to 12 weeks) if available. Maintenance study outcomes are reported at 6 months, 8-12 months, and "prolonged followup" of the final endpoint. In forest plots, outcomes in studies assessed as having a high risk of bias, or low to moderate risk of bias but at least 40 percent attrition, were presented in grey scale. Strength of Evidence for Major Comparisons and Outcomes the overall strength of evidence for primary outcomes within each comparison were evaluated based on four required domains: (1) study limitations (risk of bias); (2) directness (a single, direct link between intervention and outcome); (3) consistency (similarity of effect direction and size); and (4) precision (degree of certainty around an estimate). Assessing strength of evidence for studies with null findings is especially challenging because several domains are designed to address differences. It is hard to assess effect size when there is no effect in studies that test for superiority; how does one establish a level of precision that provides confidence of no effect This is especially true when populations, interventions, and comparators are not consistent, as is the case with much of the nondrug literature. We also downgraded precision when there was considerable attrition that was addressed through last-observation carried forward methods. Due to the large number of comparisons with findings of no effect, we assessed strength of evidence and formulated results cautiously. Based on these factors, the overall evidence for each outcome was rated as:21 High: Very confident that estimate of effect lies close to true effect. Moderate: Moderately confidence that estimate of effect lies close to true effect. Some deficiencies in body of evidence; findings likely to be stable, but some doubt. Low: Limited confidence that estimate of effect lies close to true effect; major or numerous deficiencies in body of evidence. Additional evidence necessary before concluding that findings are stable or that estimate of effect is close to true effect. Insufficient: No evidence, unable to estimate an effect, or no confidence in estimate of effect. We assessed strength of evidence for validated scales (such as the Beck Depression Inventory, Young Mania Rating Scale, Hamilton Depression Rating Scale, Clinical Global Improvement Scale) and commonly used items that examine improved function (such as the Functional Assessment Short Test). We did not assess strength of evidence for less commonly measured items such as increased time between episodes or hospitalizations. Attempted suicide and other self-harming behaviors were also not assessed for strength of evidence due to the difficulty of defining and measuring such behaviors. Bipolar research generally draws from highly defined populations, resulting in samples that are often drawn from subpopulations rather than the bipolar populations at large. Applicability also deals with transportability of evidence for the type of treatment-level of treatment, treatment fidelity, skills of treatment agent, setting (and measurement)-and its fit to a particular treatment setting. Study characteristics that may affect applicability include, but are not limited to , the population from which the study participants are enrolled, diagnostic assessment processes, narrow eligibility criteria, and patient and intervention characteristics different than those described by population studies of bipolar disorder. We addressed all reviewer comments, revised the text as appropriate, and documented all responses in a disposition of comments report made available within 3 months of the Agency posting the final systematic review on the Effective Health Care website. Literature flow diagram We identified 188 unique publications eligible for inclusion, including 123 studies of drug treatments and their associated harms, and 65 focused on psychosocial and other physical treatments. An additional 62 publications, 57 drug and 5 psychosocial, were excluded for attrition greater than 50 percent; brief abstracts of these studies are provided in Appendix D. These treatments and their comparators may have been single drug therapies or combination therapies of multiple drugs tested against either monotherapies or other multiple drug therapies. These then separated into 103 treatment comparisons, 59 of which had only one study contribute information. For Key Question 3, we found no studies meeting inclusion criteria that looked at treatments to reduce metabolic change side effects of drug treatments. Table 4 breaks the included studies down into each individual comparison for drug studies. Each study represented a unique comparison due to differences in the structure of each intervention and control/comparator groups. Table 5 provides the included studies for each individual comparison for nondrug studies. Drug Treatments for Acute Mania We identified 71 publications of 67 unique studies for acute mania that examined 28 separate drugs tested against 14 different comparators. These treatments and their comparators may have been single drug therapies or combination therapies of multiple drugs tested against either placebo monotherapies or other multiple drug therapies. The 67 studies combined into 56 treatment comparisons, 35 of which had only one study contribute information. The high attrition studies (greater than 50% were excluded because observed results among patients who complete a trial may not generalize to the entire patient population of interest if systematic differences between patients who do not complete the study and those who do. Moreover, if there are differential rates of attrition across study arms, or even similar rates but a different distribution of reasons for attrition, primary effect estimates and statistical inference can suffer from bias, potentially severe. Moreover, estimates of standard errors will understate the true uncertainty surrounding effect estimates due to the added uncertainty of having to impute data, leading readers to believe the result is more precise than it actually is and potentially inflating the type-I error rate. The results in this chapter for treatments for acute mania are organized by general drug category: antipsychotics, mood stabilizers, and drugs otherwise not specified. Within the antipsychotics section, results are presented by specific drug, then broken into single drugs compared to placebo or another drug, then, when appropriate, drug in combination with mood stabilizers compared to placebo or another drug. Likewise, the mood stabilizers and other drugs sections are presented first by single drug results followed by combination therapy results. Studies for antipsychotics plus mood stabilizers were even more sparse and scattered. The ability to draw stronger conclusions for antipsychotics was hindered by high attrition rates. Participants using atypical antipsychotics, except quetiapine, reported experiencing more extrapyramidal symptoms compared to placebo. Participants using haloperidol reported experiencing more extrapyramidal symptoms compared to other antipsychotics. Participants using olanzapine reported experiencing more clinically significant weight gain. An additional unpublished study for aripiprazole plus mood stabilizers was also included for metaanalysis. All were examined as single drugs and all but cariprazine were also examined as a treatment combined with mood stabilizers. The large majority of studies with usable outcomes were measured at 3 weeks duration. Appendix E provides detailed evidence tables, summary risk of bias assessments, forest plots when appropriate, and assessments of strength of evidence for key comparisons and outcomes. A summary of findings with at least low-strength evidence for drug treatments for acute mania are provided in Table 6. Any intervention and comparison not listed in Table 6, or outcome not listed for an included intervention and comparison, was found to have an evidence base insufficient to draw conclusions. Three studies compared aripiprazole to placebo48-50 and two compared to haloperidol. Aripiprazole Alone Table 7 summarizes the population and major inclusion and exclusion criteria for each aripiprazole study for acute mania. If fixed effect models are used, which only allows inferences for the specific participants in the specific studies, symptom improvements were seen. Akathisia and extrapyramidal symptoms were reported lower in participants using aripiprazole versus haloperidol; other harms or withdrawal outcomes were mixed. Aripiprazole Plus Mood Stabilizers Table 8 summarizes the bipolar type and major inclusion and exclusion criteria for each aripiprazole plus mood stabilizers study for acute mania. Both studies reported no differences between groups in withdrawal rates, serious adverse events, or rates of akathisia. Participants using aripiprazole reported experiencing more weight gain while participants using haloperidol reported experiencing more extrapyramidal symptoms. Asenapine Alone Table 9 summarizes the bipolar type and major inclusion and exclusion criteria for each study of asenapine alone for acute mania. We found low-strength evidence that asenapine had a lower rate of withdrawal due to lack of efficacy than placebo (moderate study limitations, imprecision). However, low-strength evidence also showed that placebo had a lower rate of withdrawal due to adverse events than asenapine (moderate study limitations, imprecision). Overall withdrawal was less in the asenapine group, and favored asenapine over placebo, but results were not statistically significant. There were no differences between groups for serious adverse events, although participants with asenapine had significantly more extrapyramidal symptoms than those on placebo. Serious adverse events were not different between arms, although participants using asenapine tended to withdraw at higher rates. Table 11 summarizes the bipolar type and major inclusion and exclusion criteria for each study. There were no differences between groups for serious adverse events, although participants using cariprazine had more extrapyramidal symptoms than those using placebo. An additional sixteen studies were excluded for greater than 50 percent attrition. Two studies of olanzapine with mood stabilizers did not use a placebo in place of olanzapine. Low-strength evidence (moderate study limitations, imprecision) also showed overall withdrawal and withdrawal due to lack of effect were lower for olanzapine. While serious adverse events did not differ by group, participants using olanzapine reported more extrapyramidal symptoms and weight gain (at least 7 percent increase) than those using placebo. However, one study noted participants receiving olanzapine experienced more clinically important weight gain (at least 7%) than those receiving divalproex;33 a trend toward greater weight gain in olanzapine groups was noted in the other studies as well. However, participants using olanzapine reported more weight gain while participants using haloperidol reported more akathisia. Results for olanzapine versus asenapine were reported in the asenapine versus active comparator section above. Olanzapine Plus Mood Stabilizers Table 13 summarizes bipolar type and major inclusion and exclusion criteria for each olanzapine plus mood stabilizers study for acute mania. Two studies examined olanzapine plus carbamazepine (n=118)70 or lithium/valproate (n=344). Two other studies examined olanzapine plus divalproex (n=202)69 or valproate (n=80)46 compared to the mood stabilizer alone without a placebo present. One study reporting response and remission rates reported results favoring olanzapine, while both reported improvements in mania symptoms. Participants receiving olanzapine reported greater frequency of clinically important weight gain. No differences were noted in serious adverse events or clinically significant weight gain. Withdrawal due to lack of efficacy was lower for quetiapine but overall withdrawal and withdrawal due to adverse events did not differ between groups (low-strength, n=1,007). Most studies reported no serious adverse events and no differences between groups for extrapyramidal symptoms. Participants using haloperidol reported more extrapyramidal symptoms; otherwise, no differences in serious adverse events were noted. Quetiapine Plus Mood Stabilizers Table 15 summarizes bipolar type and major inclusion and exclusion criteria for each quetiapine plus mood stabilizers study for acute mania. Both studies reported no differences between groups in withdrawal rates and serious adverse events, and results for extrapyramidal symptoms were mixed. Risperidone Alone Table 16 summarizes the bipolar type and major inclusion and exclusion criteria for each study of risperidone alone for acute mania. However, participants using risperidone experienced more extrapyramidal symptoms than those using placebo. Risperidone Alone Versus Active Control Evidence was insufficient for all outcomes to address whether risperidone performed better than an active comparator for acute mania, due to moderate study limitations, inconsistency, and imprecision. One study compared risperidone to lithium, finding no difference between groups in bipolar outcomes and extrapyramidal symptoms at 4 weeks. Results for risperidone versus olanzapine were reported in the olanzapine versus active comparator section above and were determined to yield insufficient evidence. Risperidone Plus Mood Stabilizers Table 17 summarizes bipolar type and major inclusion and exclusion criteria for each risperidone plus mood stabilizers study for acute mania. No differences were reported in adverse events; however, participants using risperidone experienced more extrapyramidal symptoms. Ziprasidone Alone Table 18 summarizes the bipolar type and major inclusion and exclusion criteria for each study of ziprasidone alone for acute mania. Withdrawal due to lack of effect also was lower for the ziprasidone group, while no differences were seen for overall withdrawal or adverse events. Serious adverse events were reported in one study, with no difference between groups. However, in one study participants using ziprasidone experienced more extrapyramidal symptoms than those using placebo. No differences were reported in adverse events, however participants using high dose ziprasidone experienced more extrapyramidal symptoms. Haloperidol Alone Table 20 summarizes the bipolar type and major inclusion and exclusion criteria for each study.

Summary Follow-up period Due to the novelty of such procedures metabolic disease center amaryl 2mg lowest price, few data are available with regard to mid-term and long-term patency rates [12-15] diabetes diet sugar order amaryl 4mg mastercard. In our first patient diabetes mellitus osmotic pressure buy cheap amaryl on-line, whose operation was performed in October 2002 diabetes symptoms 9 year old buy generic amaryl 1 mg, continued enlargement of the aneurysm sac was observed in 2004 diabetes medicine of himalaya buy cheap amaryl 1 mg on-line, although no endoleak was detected diabetes type 1 child order amaryl 4mg free shipping. Interestingly, we have observed this phenomenon in two other patients who received Excluder stent-grafts to treat degenerative chronic descending thoracic aortic aneurysms. The mechanism remains speculative, however, type V endoleaks remain the most likely cause of this phenomenon. All three of these All reports available in the literature to date confirm the safety and efficacy of supra-aortic reconstructions (using both autologous approaches and synthetic grafts) with subsequent stent-graft placement to exclude aortic arch aneurysms in patients not suitable for conventional surgical repair. In our experience, the autologous transposition procedure can be performed safely without exposing these elderly patients, who are frail and have a diminished physiologic reserve, to substantial risk. Synthetic grafts can be used when endograft coverage needs to be extended to the innominate artery. The increasing experience with combined approaches for arch aneurysms will undoubtedly extend the indications for using stent-grafts in this delicate anatomic region. In fact, a variety of new adjunctive techniques to enable stent-graft placement in patients with arch aneurysms are rapidly becoming available. An alternative procedure of endovascular stent-graft repair for distal arch aortic aneurysm involving arch vessels. Combined repair of an aortic arch aneurysm by sequential transposition of the supraaortic branches and consecutive endovascular stent-graft placement. Initial results after combined repair of aortic arch aneurysms by sequential transposition of the supra-aortic branches and consecutive endovascular stent-graft placement. Surgical treatment of an aortic arch aneurysm without cardiopulmonary bypass: endovascular stent-grafting after extraanatomic bypass of supra-aortic vessels. An alternative approach in treating an aortic arch aneurysm with an anatomic variant by supraaortic reconstruction and stent-graft placement. Cryopreserved vascular allograft in the treatment of major vascular infection: a comparison with conventional surgical techniques. Nature and significance of endoleaks and endoextension: summary of opinions expressed at an international conference. Longitudinal aneurysm shrinkage following endovascular aortic aneurysm repair: a source of intermediate and late complications. The need for clinical trials of endovascular abdominal aortic aneurysm repair: the Eurostar Project. Human cytokine responses to coronary artery bypass grafting with and without cardiopulmonary bypass. Inflammatory response and myocardial injury following coronary artery bypass grafting with or without cardiopulmonary bypass. Endovascular stent-graft repair of complicated penetrating atherosclerotic ulcers of the descending thoracic aorta. Technical strategies to expand stent-graft applicability in the aortic arch and proximal descending thoracic aorta. However, several factors interact to precipitate bleeding in patients who undergo aortic arch repair, arguably making it more difficult to achieve effective hemostasis during these operations than in any other type of cardiovascular procedure. One such factor is the long suture lines that aortic arch repairs often require; portions of these lines become difficult to access once the repair is complete, and they involve aortic tissue that is extremely fragile, especially in patients with acute aortic dissection or connective tissue disorders. Additionally, aortic arch operations are often complicated by coagulopathy, which may arise from the use of hypothermic circulatory arrest and the large transfusion requirements associated with the procedure. Several surgical adhesives have been developed to improve hemostasis by reinforcing suture lines and repairing fragile tissue. All of these agents can act as sealants, forming a hemostatic coating over tissues; some also produce strong bonds between juxtaposed tissues. The different types of surgical adhesives that have been used to improve hemostasis during cardiovascular operations include aldehyde-based glues, fibrin sealants, collagenbased adhesives, polyethylene glycol polymers (hydrogels), and cyanoacrylates [1-5]; however, only two of these - aldehyde-based adhesives and fibrin sealants - have been widely used to facilitate aortic arch repairs. Aldehyde-based glues Aldehyde-based glues create strong bonds by crosslinking proteins. Because these glues have excellent adhesive strengths [6], they are particularly useful for bonding the layers of the dissected aorta together and reinforcing aortic tissue weakened by age or disease. This glue is a two-component aqueous system that undergoes a reaction to form a water-insoluble crosslinked resin. One component of the system is the formaldehyde/glutaraldehyde mixture; the other component is a solution of gelatin, resorcinol, and calcium chloride. First, it may cause tissue toxicity because of the high concentration of formaldehyde. BioGlue surgical adhesive is a two-component, aldehyde-based glue that has become widely available. BioGlue is composed of 45% purified bovine serum albumin and 10% glutaraldehyde, which mix within the delivery tip during application. Compared with other surgical adhesives and sealants, BioGlue demonstrates excellent tensile and shear strengths. Also, because BioGlue is stored and used at room temperature and requires no solution preparation before use, this product offers the advantage of immediate availability. Many groups use balloon catheters to compress the layers and obtain an adequate seal [10,12,13] or use forceps or special clamps to seal the layers together during bonding [9]. The adventitial inversion (or `cul-de-sac`) technique, whereby the edge of the outer layer of the aorta is folded into the true lumen to further seal the false lumen, is used in conjunction with glue by some [13]. The use of felt as additional reinforcement varies substantially among surgeons: some avoid using felt altogether [14], whereas others use felt strips both inside and outside the aorta [9,15], place felt inside the false lumen [16], or wrap felt circumferentially around the aorta [12]. Despite these limitations, fibrin sealants have been shown to effectively reduce bleeding from tissue surfaces and anastomoses [20], and these adhesives have been used safely during acute aortic dissection repairs [6,21]. Nakajima and colleagues [22] recently described a technique in which a sheet of knitted polyester fabric is soaked in the fibrinogen solution and inserted between the dissected layers of the aorta, the thrombin solution is added on each side, and the layers are compressed, effectively obliterating the false lumen. Balancing risks and benefits Although surgical adhesives offer the opportunity to improve patient outcomes, these agents can cause early and long-term complications; therefore, improving their safety by carefully defining and addressing potential problems is essential. The critical balance between maximizing benefit and minimizing risk should be evaluated for each individual patient. Many groups have reported subjective benefits of using adhesives to facilitate aortic repairs. Adhesives appear to improve hemostasis, strengthen weak tissues, provide anastomotic support, and enhance the durability of repair [23-25]; these benefits are especially pronounced in patients with marked tissue fragility, including those with acute dissection or connective tissue disorders. Additional purported early benefits of adhesive use include reduced bleeding, decreased transfusion requirements, shortened operative and circulatory arrest times, and shortened lengths of hospital stay [21,23,26]. Additionally, the reduction in intra-operative bleeding could, theoretically, minimize the risk of coagulopathy and the need for early reoperation [17]. Whether adhesives provide longterm benefits, such as a reduced incidence of false lumen patency and a decreased incidence of late reoperation, remains controversial [9,27-29]. Although surgical adhesives may offer benefits, they pose several potential risks that warrant attention. Allergic reactions and infectious disease transmission remain concerns when one is using products of bovine or human origin. Additionally, the aldehyde components of adhesives have been reported to be directly toxic to nerves [30-33]; thus, when using aldehyde-based adhesives during arch repair, surgeons should take extra care to avoid the nearby phrenic and recurrent laryngeal nerves. The concerns about tissue toxicity in nerves also apply to cardiac conduction tissue [32,34]. Fibrin sealants vary in their composition but generally include a fibrinogen solution (fibrinogen + fibrinolytic inhibitor) and a thrombin solution (thrombin + calcium chloride solution). When the two components are mixed at the site of use, the gel solidifies in a reaction mimicking the physiologic coagulation and tissue adhesion cascade. The biologic components can potentially transmit infectious diseases, although aggressive pathogen inactivation protocols are used to minimize this risk. Systems that prepare autologous fibrin sealant promise to improve biocompatibility and eliminate the risks of viral infection [18,19], but such systems are not widely used. Further, fibrin sealants do not bond as strongly as aldehyde-based adhesives and may be weakened through fibrinolysis. Reports after reoperations have described necrotic, fibrosed, and excessively thinned aortic tissue found at the site of adhesive application [27,35,37,39,41]. Because aldehydebased glues have been linked to the development of vascular strictures and impaired aortic growth, they are not recommended for use during cardiovascular reconstructions in pediatric patients [35,41]. Systemic embolization of adhesive fragments is another concern, especially given the proximity of the brachiocephalic vessels during aortic arch repair. Some authors have used adhesive in the brachiocephalic vessels when dissection is present [42]; this should be done with caution because of the potential for embolization. Several reports have raised concerns about adhesive leaking into the aortic lumen, resulting in valve dysfunction or embolization [43-47]. Cerebral and myocardial infarctions caused by polymerized glue emboli have been found on autopsy, and polymerized glue emboli have been extracted from patients with severe acute limb ischemia [45,47,49]. Carrell and associates [49] have suggested three mechanisms by which adhesives may cause embolization: direct spillage into the true lumen (despite precautions), escape through reentry sites into the true lumen, and leakage through suture-line needle holes. The first two mechanisms can result from technical error, so careful attention and proper training of the surgical team will minimize this risk. Fortunately, the number of reported cases involving adhesive embolization remains low; however, the incidence of adhesive embolization may be underestimated, because adhesive embolization is rarely suspected as a cause when ischemic complications arise and because post-mortem microscopy examinations are not routinely performed in patients that succumb to complications of cardiovascular repairs. Given the well-documented risks involved in using surgical adhesives during aortic repairs, we do not recommend doing this routinely; however, during certain complex operations - especially in cases of acute aortic dissection - the benefits of using these agents may truly outweigh the potential risks. Thus, the risk-benefit ratio for using glue should be carefully considered on a patientby-patient basis. Adhesives and sealants should be used only when medically necessary to secure hemostasis and reinforce weak tissues. When the use of surgical adhesive is warranted by the clinical situation, several technical considerations can be applied to make the use of these products as safe as possible. Technical aspects of using glue during aortic arch repair We primarily use BioGlue in patients with acute aortic dissection; we perform these procedures using profound hypothermic circulatory arrest and an open distal anastomosis [51]. BioGlue is used to obliterate the false lumen and reinforce the fragile suture lines. Because blood interferes with tissue bonding, all clotted and fresh blood is removed from the false lumen to create a dry field. It is also sometimes necessary to stop antegrade or retrograde cerebral perfusion briefly before glue is applied. The dissecting membrane is carefully tacked to the outer wall with a few interrupted 6-0 sutures to keep the walls aligned during glue application. To protect surrounding structures from the tissue and nerve damage that contact with the glue can cause, gauze sponges dampened with saline can be used to shield these tissues from unintentional adhesive run-off during glue application. A Foley catheter with a 30-cc balloon is inserted via the true lumen into the proximal descending thoracic aorta, immediately distal to the left subclavian artery, and inflated to prevent the adhesive from running down the false lumen into the descending thoracic and abdominal aorta. Avoiding the distal run-off of glue also keeps the adhesive in the arch, thus maximizing bonding and preventing distal embolization through the false lumen [48]. Additionally, a moist sponge can be placed in the true lumen to cover the origins of the brachiocephalic arteries and prevent any adhesive that spills over the edge of the dissecting membrane from running into these vessels. Before BioGlue is applied, the applicator tip is primed to evacuate air and ensure the proper mixing of the components. This adhesive has a very low viscosity, making it difficult to fully control during application, particularly if it is rapidly released. Slowly releasing the glue during application tends to increase its initial viscosity and improve control. BioGlue is released so that a thin (~2 mm) layer fills the false lumen, while spillage outside the aorta or into the true lumen is carefully avoided. Any spilled adhesive is rapidly evacuated with the wall suction (never with the cell saver or pump suctions). The walls of the aorta do not need to be pressed together; in fact, the goal is to maintain an even layer of glue between the tissue layers as it bonds to the aorta and polymerizes. The arrows indicate the direction of arterial inflow from the cardiopulmonary bypass pump. In this case, a beveled hemiarch repair is being performed during hypothermic circulatory arrest while antegrade cerebral perfusion is being delivered via a right axillary artery cannula. Note the fine sutures that keep the dissected layers of the aorta aligned, the inflated balloon catheter in the proximal descending thoracic aorta, and the protective moist sponge inside the true lumen. Because the glue requires a dry field to properly set, cerebral perfusion is often briefly stopped while the glue is applied. A thin layer of glue is applied to the suture line after this anastomosis is completed, before systemic perfusion is resumed. Note the fine sutures keeping the layers of the aorta aligned, and the protective moist sponge covering the aortic valve and coronary ostia. We do not incorporate felt strips into the anastomosis; however, after completing the suture line, we routinely use pledgeted mattress sutures to circumferentially reinforce the anastomosis. We then apply a thin layer of BioGlue to the outer surface of the distal suture line before restoring arch perfusion and proceeding with the proximal portion of the repair. After the glue has set, the proximal anastomosis is performed and reinforced with pledgeted mattress sutures. A thin layer of BioGlue is applied to the completed anastomosis before the aorta is unclamped; to reduce the chance of glue leaking into the lumen while being applied to the suture line, it is important to temporarily stop the left ventricular sump suction [50]. We occasionally also use BioGlue when repairing aortic arch aneurysms in patients without acute dissection.
Pathophysiology the pathophysiological effect depends on the size of the tunnel and the amount of regurgitation managing diabetes 88 purchase amaryl 2mg on-line. But almost all have aortic valve regurgitation or signs of left ventricular dilatation and hypertrophy diabetes in dogs side effects of insulin amaryl 1mg with visa. While many patients may have no symptoms diabetes test how to order amaryl on line amex, others may pre sent with rapid progression or sudden death www.diabetes diet.co.za purchase amaryl online pills. The symptoms are dependant on the size of tunnel diabetes type 2 levels purchase cheap amaryl, its hemodynamic influence and the associated cardiac defects diabetes mellitus type 2 causes buy discount amaryl 4mg online. It is usually accompanied by systolic and diastolic thrills felt on a wide area on the precordium. In those with a tunnel, with associated severe aortic valve obstruction, heart failure occurs early, with or without low cardiac output and nearly one third of reported cases having died before birth or on the first day of life. The middle figure shows a cross-sectional view at the approximate level of the aortic sinotubular junction. The tunnel passes from the ascending aorta into the tissue plane between the aortic and pulmonary roots. In this example, the aortic end of the tunnel lies above the ostium of the right coronary artery, while the ventricular end is found within the intercoronary, interleaflet triangle. The position of the aortic opening is variable and may be found anywhere above the left or right coronary sinus, or the intervening commissure. Because the pulmonary valve lies distal to the aortic valve, the tunnel may displace the free-standing, muscular, sub-pulmonary infundibulum enroute to the left ventricular cavity. In some patients, the tunnel itself can be seen as a leftward prominence of the aortic root in the area of the pulmonary trunk. A B figures 3A and B: Echocardiogram with color Doppler in an 11 month infant with aorto-right ventricular tunnel: A. Apical five-chamber view shows the dilated tunnel arising from the right aortic sinus; B. Parasternal short-axis view shows normal sized left and right coronary arteries arising from left coronary sinus. On color Doppler studies, diastolic flow is seen passing from the aorta to the left ventricle and systolic from the ventricle to the aorta. Cardiac catheterization with angiography is now indicated only when associated lesions or coronary arterial origins cannot be evaluated with certainty on noninvasive studies or when percutaneous intervention is planned. Of all these features, extensive and uniform dilation of the ascending aorta may be the best noninvasive clue to the diagnosis of aortoventricular tunnel, for this is hardly ever present early in life with other cardiac malformations. Extremely rarely enlargement of the aorta is not present, specifically when there is critical obstruction of both the aortic valve and within the tunnel. Echocardiogram in parasternal long-axis shows tunnel arising from aorta entering into the left ventricle; B. Computed tomography angiogram shows the dilated tunnel arising from right sinus with right coronary artery and left coronary artery (branching into left anterior descending and circumflex arteries) arising from left coronary sinus (three white arrows) B. Apparent aortic regurgitation which is extremely uncommon during fetal life and enlargement of the aortic root, further supports a diagnosis of aortoventricular tunnel. The flow while flow of blood around the hinge of the valve can also be imaged with color flow Doppler echocardiography. The key to diagnosis in fetal life is aortic regurgitation, sometimes with left ventricular dysfunction and hydrops. If they present in infancy in congestive heart failure, medical management results in almost 100 percent mortality, usually soon after presentation. These include rupture of sinus of Valsalva aneurysm, truncus arteriosus with valvular regurgitation, aortopulmonary window, ventricular septal defect with aortic regurgitation, patent ductus arteriosus, coronary cameral fistula, valvar aortic stenosis and regurgitation, tetralogy of Fallot with absent pulmonary valve and cerebral arterio venous malformation. Both the left and right coronaries are seen arising from the left coronary sinus; B. The tunnels between the aorta and the left atrium is extremely rare and is more often associated with complications of infective endocarditis65 and paravalvular abscess, aortic dissection66 and after surgery affecting the valve or aortic root. Due to the benefit of providing support for the aortic valvar leaflets, as well as the spectrum of associated coronary arterial anomalies, it seems likely that repair of the aortoventricular tunnels should remain largely, if not exclusively, within the surgical domain as it is questionable Aorta-right Atrial tunnel the aortaright atrial tunnel was first described in 1980. The tunnel originating in the left sinus of Valsalva usually has a posterior course whereas, the tunnel from right sinus of Valsalva, has an anterior course before joining the right atrium. Associated conditions with this anomaly are secundum type of atrial septal defect and persistence of the left superior vena cava. These are attributable either to an aneurysmal dilation of the sinus nodal artery or to a congenital weakness of the elastic lamina in the aortic media. Aortic root angiogram shows dilated aortic root with moderate aortic regurgitation and aneurysmally dilated extracardiac portion of tunnel entering the left ventricle; B. Most patients may be asymptomatic or they may present with exertional breathlessness, palpitations or recurrent respiratory tract infections. Rupture of sinus of Valsalva can be differentiated by demonstrating a tunnel with an extracardiac course. Electron beam tomography can be a good diagnostic tool, showing the tunnel taking its origin from the aortic root and entering the right atrium through a tortuous communication. Moreover, the continued patency of the tunnel leads to risk for biventricular volume overload, bacterial endocarditis, pulmonary vascular disease, aneurysm formation, calcification of the wall, aortic regurgitation and spontaneous rupture. They include transcatheter closure, ligation under controlled hypotension or repair with the patient under under cardio pulmonary bypass. The ligation for anteriorly located aortaright atrial tunnel includes ligation near the aortic end, and for posteriorly located tunnels, ligation should be done between between superior vena cava and aorta as close to the aorta as possible. Surgical closure of tunnel along with repair of the associated cardiac defects has been achieved with satisfactory results in the past. Multiple aorticocameral tunnels associated with bicuspid aortic valve in aged: a case report. The pathological anatomy of deficiencies between the aortic root and the heart, including aortic sinus aneurysms. Aortico-right ventricular tunnel with critical pulmonary stenosis: Diagnosis by two dimensional and Doppler echocardiography and angiography. Aorta right ventricular tunnel with a rudimentary valve and an anomalous origin of the left coronary artery. Repair of aortoright ventricular tunnel with pulmonary stenosis and an anomalous origin of left coronary artery. Transcatheter closure of a rare case of aortoright ventricular tunnel with single coronary artery. Repair of aorticoleft ventricular tunnel in the neonate: surgical, anatomic and echocardiographic considerations. Aortico-left ventricular tunnel: a clinical review and new surgical classification. Aortic atresia and aortico-left ventricular tunnel: successful surgical management by Konno aortoventriculoplasty in a neonate. Aortico-right ventricular tunnel and critical pulmonary stenosis: diagnosis by twodimensional and Doppler echocardiography and angiography. Repair of aorticoleft ventricular tunnel associated with subpulmonary obstruction. Aortico-left ventricular tunnel with ventricular septal defect: two-dimensional/ Doppler echocardiographic diagnosis. Correction of aortico-left ventricular tunnel in a small Oriental infant: a brief clinical review. Aortic left ventricular tunnel: Successful diagnostic and surgical approach to the oldest patient in the literature. Two-dimensional echocardiographic identification of aortico-left ventricular tunnel. Aortico-left ventricular tunnel: diagnosis based on two-dimensional echocardiography, color flow Doppler imaging, and magnetic resonance imaging. Twodimensional and realtime threedimensional echocardiographic fetal diagnosis of aorto-ventricular tunnel. Aortic atresia with aorticoleft ventricular tunnel mimicking severe aortic incompe tence in utero. Aortic-left ventricular tunnel associated with critical aortic stenosis in the newborn. Right coronary artery from aorto-left ventricular tunnel: case report of a new surgical approach. Aorto-left ventricular tunnel: transcatheter closure using an amplatzer duct occluder device. Use of an Amplatzer duct occluder for closing an aorticoleft ventricular tunnel in a case of noncompaction of the left ventricle. Aortic dissection with aorto-left atrial fistula formation soon after aortic valve 23 AorticocAmerAl tunnelS 345 4 Shunt DefectS 67. Aorta right atrial tunnel: clinical presentation, diagnostic criteria, and surgical options. Congenital aorta right atrial fistula: successful transcatheter closure with the Amplatzer occluder. Aorta to Right Atrial Tunnel: Prenatal Diagnosis and Transcatheter Management in a Neonate J. Coarctation of the aorta, atrial septal defect, tetralogy of Fallot and patent ductus arteriosus also may be associated with these aneurysms. Two-thirds of the aneurysms are located in the right aortic sinus, one-fourth in the noncoronary sinus and the rest in the left aortic sinus. Rarely, rupture is into the pulmonary artery,12-14 left ventricle,15-17 left atrium17 or pericardial cavity. It often ruptures into the right atrium and sometimes into the right ventricle, just below the septal leaflet of the tricuspid valve. The apical four-chamber view shows dilation of the left ventricle and left atrium, with the aneurysm of the right sinus of Valsalva burrowing into the ventricular septum. The apical five chamber view shows the aneurysmally dilated left sinus of Valsalva prolapsing into left ventricle, producing saccular protrusions and aortic regurgitation. Depending on the chamber, which receives the ruptured blood, both right and left side of the heart is under volume overload, which if large and sudden can lead to congestive heart failure. Aneurysm rupturing into right atrium causes volume overloading of all four chambers. Occasionally, unruptured aneurysms can produce symptoms of intractable angina because of distortion of the origin of the coronary arteries. Although rupture has been reported in the neonatal period,31 it occurs more frequently in the third or fourth decade of life. The sudden onset of dyspnea rather than pain or mild chest pain may occur for weeks before the onset of dyspnea and tightness in the upper abdomen. Occasionally, the aneurysm compresses a coronary artery so symptoms of myocardial ischemia or infarction coexist. Transthoracic echocardiographic parasternal long axis view shows aneurysms of both aortic coronary sinuses of Valsalva obstructing the left ventricular outflow tract. Parasternal short-axis view shows the aneurysm of the right sinus protruding into the right ventricular outflow tract. Ruptured aortic sinus aneurysms typically express themselves in young men after puberty, but before the age of 30 years. The physiologic consequences of rupture depend on three factors: 348 When chest pain, dyspnea and a continuous murmur suddenly develops in a patient with a ventricular septal defect, the reason is likely to be rupture of a coexisting aortic sinus aneurysm. If the fistula enters the right side, there will be right ventricular hyperactivity as well. Occasionally, there is only a diastolic murmur in fistulas entering the left ventricle9 or the high-pressure right ventricle in a neonate. Myocardial infarction may be the consequence of compression of the coronary arteries and may occasionally be fatal. Atrioventricular conduction defects including complete heart block and right or left bundle branch block or bifascicular block5,43 result when a ruptured or unruptured aneurysm penetrates the base of the ventricular septum. Volume overload of both ventricles with congestive heart failure accounts for the radiologic picture when an aortic sinus aneurysm ruptures into the right side of the heart. Large rupture causes pulmonary venous congestion because of sudden rise in end diastolic pressure of an unprepared left ventricle, and also prominence of pulmonary trunk because of increased pulmonary blood flow. Occasionally right or left aortic sinus aneurysm may project out as dense convex paracardiac shadow. Unruptured defects are characterized by phasic expansion and relaxation and to-and-fro pulsed Doppler signals at the site of origin from the aorta, but no color flow evidence of rupture. Continuous systolic and diastolic turbulence detected by the pulsed wave Doppler just distal to the area of perforation at high velocities. Color flow mapping with mosaic turbulence across the perforated aneurysm in real time. Ischemic left ventricular regional wall motion abnormalities caused by compression of the coronary artery origins by the aneurysm are evident on real time screening. Non-invasive imaging with computed tomography or magnetic resonance scans have been shown to provide excellent definition of the aneurysm and the tissue planes involved. Surgical treatment is necessary, if the size of the aneurysm is larger than 50% of the average size of the other two normal Valsalva sinuses or is increasing in consecutive echocardiographic examinations. In addition, patients should be operated on if there is compression or malformation of the adjacent tissues. Although, the mortality is low (< 2%), the potential morbidity from cardiopulmonary bypass and thoracotomy including the scar are the underlying hazards. Although the long-term result of the successful repair is usually good, residual shunt may require reoperation, which carries a high mortality. Patient with left-to-right shunt with pulmonary to systemic flow ratio of greater than 1. The procedure is performed under local anesthesia with fluoroscopic and transthoracic/transesophageal echocardiographic guidance. After establishing femoral artery and venous access, intravenous antibiotics and heparin is given at 100 mg/kg, right and left heart catheterization is done, and direct pulmonary artery pressure is measured.

Tissue microarray detection of matrix metalloproteinases in diseased tricuspid and bicuspid aortic valves with or without pathology of the ascending aorta diabetic humor buy cheap amaryl online. They are superior in evaluating the aortic wall and periaortic space for pleural and pericardial effusions and are approaching conventional angiography in evaluating the aortic lumen diabetes injectable medications list discount amaryl 4 mg amex. Catheter-based angiography diabetic diet recipes menus buy 1 mg amaryl fast delivery, despite being invasive and more costly diabetes medications types purchase amaryl toronto, will continue to play a complementary diagnostic role in selected cases diabetes in dogs books purchase amaryl online pills. It is more sensitive in the detection of small branch vessel disease diabetes test cost in india buy discount amaryl on line, and in evaluating flow dynamics and collateral vessel pathways. It is important to be able to correlate angiographic findings with cross-sectional imaging, particularly as catheter-based minimally invasive therapy becomes more prevalent. In this chapter, we will examine technical and anatomical considerations as well as the role of angiography in the diagnosis of various disease processes. Furthermore, images are immediately available for display in the operating suite or viewing via web-based distribution to remote sites. Thoracic aortography is performed utilizing standard Seldinger technique via the femoral artery approach. A multi-side-hole catheter, usually of the pigtail configuration, is advanced over a guidewire adjacent to the aortic valve to ensure complete aortic evaluation. Injection of 50-60 ml of low osmolarity contrast over two seconds with acquisition rates of 3-5 images per second are standard. It is important for patients to remain motionless during image acquisition - any motion will significantly degrade image quality. Serious complications are fortunately uncommon, usually related to puncture site problems (hematoma, pseudoaneursym) that occur in less than 5% of procedures, and are decreasing secondary to use of smaller catheters and puncture site closure devices. Arterial thrombosis, perforation, dissection and distal embolization are similarly unusual. The incidence of stroke with non-selective aortography is extremely low (<1%) and has not been seen by the authors. Typically, the risk of contrast-induced nephrotoxicity is minimized by the use of non-ionic low osmolarity contrast agents (iodixanol 270 mgI/ml and iohexol 300 mg/ml) and ensuring adequate hydration before and after the procedure (100 ml normal saline per hour for six hours before and after the procedure). The administration of acetylcysteine (600 mg by mouth twice a day, the day before and the day of the exam) and dopamine (2. For patients with a history of mild-to-moderate (non-anaphylactic) contrast allergy, premedication with H1-blockers and oral steroids minimizes the severity and frequency of adverse reactions (diphenhydramine 50 mg by mouth and prednisone 50 mg by mouth, 12 and 2 hours prior to scheduled time of examination). Anatomy and variants With proper catheter positioning, the aortic root and coronary arteries are opacified. The diameter of the root 31 Aortic Arch Surgery: Principles, Strategies and Outcomes. In approximately 70% of individuals, the branches of the aortic arch are the innominate, left common carotid and left subclavian arteries [1,2]. The junction of the aortic arch and descending aorta is called the isthmus and is the site of the involuted ductus arteriosus. The posterior intercostal, esophageal and bronchial arteries are smaller branches that arise directly from the thoracic aorta. A detailed discussion of vascular anomalies related to embryonic errors of involution and persistence of the paired dorsal and ventral aortae is beyond the scope of this chapter and may be found elsewhere (see Chapter 2). The vessel passes posterior to the esophagus and in rare cases may cause dysphagia or massive hemoptysis when associated with vasculitis or an aneurysmal diverticulum of Kommerell [3,5,6]. Stenotic and occlusive disease Atherosclerotic disease rarely produces hemodynamically significant stenosis of the thoracic aorta. It commonly involves the proximal great vessels and may result in vascular insufficiency to the brain or upper extremities. The demonstration of the stenosis/occlusion as well as reversed vertebral blood flow on aortography is integral not only to diagnosis but subsequent therapy, either open surgical bypass or angioplasty/stenting. Coarctation is a narrowing of the aorta whose angiographic appearance depends on whether it is of the postductal (adult) or preductal (infantile) types. This patient also has a left vertebral artery (arrow) arising directly from the aorta. The preductal type is usually discovered in neonates with congestive heart failure and appears as a long segment narrowing proximal to the patent ductus arteriosus. Pressure measurements across the stenosis are helpful to confirm the severity of the narrowing and serve as an end point to endovascular therapy (dilatation/stenting). In the early stages, which are characterized by non-specific constitutional symptoms, aortography is normal. Delineation, not only of stenoses and occlusions, but also mapping of critical collateral vessel pathways is important in planning therapeutic options. Most commonly, stenoses involve long segments, are smooth, and often progress to occlusions; however, vessel dilatation and aneurysm formation may occur uncommonly. Pulmonary artery stenosis has been variably reported to occur in 33-70% of patients. Angiographically, the Ueno classification as modified by Lupi-Herrera has commonly been used (Table 4. Aneurysms may 34 be morphologically referred to as fusiform, saccular, or cylindrical. Pathologically, the integrity of all layers of the aortic wall is maintained in true aneurysms, while there is disruption of one or more of these layers in false aneurysms. On aortography, injected contrast usually discloses a dilated lumen; however, dilation of the opacified lumen may be absent in those instances where mural thrombus is present. Secondary signs of mural thrombus include a smooth aortic wall and calcification peripheral to the opacified lumen. Historically, aortic arch aneurysms have been seen as a sequel to syphilitic infection up to three decades later. Syphilitic aortic aneurysms have become exceedingly rare following the introduction of effective antibiotic therapy. Traumatic injuries to the aorta or great vessels may be related to penetrating or blunt insults and result in false aneurysms confined by periaortic soft tissues. In significant deceleration injuries, most commonly related to high-speed motor vehicle accidents, laceration of the aorta may occur. Aortic injuries are most commonly seen at the level of the isthmus (90%), followed by the proximal ascending aorta (5%), and distal descending aorta near the diaphragmatic hiatus (1-2%)[11]. Attention must also be paid to the origins of the great vessels where injuries also occur, particularly in cases of sternal, clavicular and upper rib fractures. The extent of injury can range from an intimal tear to complete transection with false aneurysm formation. Occasionally, a linear radiolucency within the false aneurysm which represents the intimal/medial flap may be seen; demonstration of active contrast extravasation is rare. Generally, the aneurysm makes an acute angle with the adjacent aortic isthmus and contrast washout is delayed. It is distinguishable by smooth margins and obtuse angles at its junction with the aorta. Mycotic aortic aneurysms account for a small (<5%) percentage of all aortic aneurysms. They are classically false aneurysms, saccular, lobulated and prone to rupture [12]. Chest X-ray may show widening of the mediastinum, disparity between the size of the ascending and descending aorta, or displacement of intimal calcification centrally. These limitations are, however, decreasing as newer generation equipment becomes more ubiquitous. Aortography can be extremely valuable in assessing for valvular insufficiency, extension into the coronary arteries and great vessels and in evaluating the abdominal aorta and visceral vessels when there are signs of mesenteric or renovascular insufficiency. Depending on the quality of peripheral pulses, a femoral artery approach from one or both groins is the preferred route of entry. Great care in advancing the guidewire should be taken; if it hangs up, the wire should be redirected by means of a steerable catheter. It is frequently possible to evaluate both the true and false lumens from a single puncture site; occasionally alternative approaches, including brachial or axillary punctures, are needed. Differential opacification of the two lumens may occur, dependent on the size and location of entry and re-entry tears, catheter positioning and the dynamic nature of the flaps during systole and diastole. Typically, the overall aortic lumen is increased in size and the larger lumen is usually the false lumen. A penetrating ulcer is a variant of dissection in which there is a breach of the intima and media related to atheromatous disease. Symptomatically, they often are painful as a result of enlargement of the ulcer or intramural extension proximally or distally. Angiographically, they have a typical appearance when viewed in profile as a focal protrusion from the expected confines of the aortic wall in the setting of aortic wall thickening [14]. The ulcer may have smooth or lobulated margins and may undermine the intima and media when dissecting intramurally. In fact, dissections which are atypical in location, such as those localized to the arch or the distal descending thoracic aorta, may actually originate as penetrating ulcers. Diverticula of Kommerell and aberrant subclavian arteries complicated by aneurysms. Although the newest generation of angiography suites have begun to incorporate 3D and multiplanar capabilities, persisting limitations of aortography include its invasiveness and its relatively high cost. Because of these benefits and the rapidly expanding opportunities for catheter-based treatment, aortography will continue to play an important role in evaluating and managing patients with aortic arch disease. Faster scanning also yields advantages such as reduced respiratory motion artifact, cardiac gating capability, and options for imaging during multiple phases of contrast enhancement with a single contrast bolus at submillimeter collimation. For this reason, it is almost invariably the modality of choice for imaging patients with trauma and all other emergency thoracic aortic conditions. It can easily differentiate vascular from non-vascular causes of acute and chronic disease. Patients with substantial maxillofacial injuries, severe coagulopathy, history of radiation therapy to the chest and severe esophageal disease are generally excluded. Catheter-based aortography is invasive, costly and not readily available at all times. This delay is clinically relevant as it can result in increased morbidity and mortality, particularly for traumatic aortic injury and dissection. More importantly, aortography is limited to evaluation of the intraluminal component of aortic pathology, and it cannot diagnose other causes of chest pain or mediastinal widening. For practical reasons, its use has become quite limited, particularly for emergency aortic imaging. The latest model scanners are now equipped with automated techniques that determine the optimal scan delay. By sampling the enhancement of the aorta until a pre-set threshold of contrast density is reached, imaging can be triggered to occur during peak arterial enhancement. A third scan can be performed after a 60-second delay to evaluate solid and hollow abdominal visceral perfusion, and late enhancing vascular structures. For example, slow flow in a false lumen of a dissection can be mistaken for thrombosis during a single early phase of enhancement. Raw image data should be acquired and reconstructed at the thinnest practical slices for optimal 3D reconstructions. This can be useful for better defining the relationship of intraluminal aortic pathology. Small intramural hematomas, periaortic hematomas from leaking aneurysms, displaced intimal calcifications and post-surgical material can be masked or confused with high-density contrast material on enhanced scans, but are easily detected and differentiated on unenhanced scans. Even subtle detail of the ascending aorta, such as valve leaflets, coronary sinuses and vessels can be imaged and evaluated with confidence. This added information can greatly influence patient management, since a common problem in patients with ascending aortic dissection is extension into the coronary arteries. Primary evaluation of left and right main coronary artery disease can also be achieved when cardiac gating is performed as part of an evaluation for undifferentiated chest pain. It should be liberally used to reduce motion artifact resulting from ventricular systole. Routine use improves imaging and reduces the pitfalls that lead to misdiagnosis in the proximal aorta (root, ascending and arch). It is in this context that we are reminded that these diagnoses are not always mutually exclusive, as they can often coexist on a spectrum of aortic pathology. Patient characteristics such as obesity and poor cardiac output can also compromise study quality and decrease conspicuity of findings such as an intimal flap or subtle wall irregularity. Other solutions include the use of diluted contrast material or lower extremity injection, though neither is routinely employed at most institutions. The latter is least favored due to the sometimes unpredictable timing of the contrast bolus. One of the most important challenges when imaging the ascending aorta results from a combination of aortic root motion (pulsation) and z-axis blur [7]. The characteristic appearance of this left anterior, right posterior curvilinear artifact should be recognized. Normal enhancing periaortic vascular structures can simulate aortic pathology to untrained reader. In particular, the left brachiocephalic vein, left superior intercostal vein, right atrial appendage, aortic sinuses of Valsalva and left inferior pulmonary vein are normal structures that course in close proximity to the aorta and can mimic dissection. For example, an aberrant right subclavian artery sometimes reveals dilatation at its origin that can be mistaken for a post-traumatic pseudoaneurysm.
Septum secundum diabetes diet menu pdf discount amaryl 4mg free shipping, on the other hand diabetes type 2 what not to eat buy amaryl online from canada, develops through enfolding of the roof of the atrium to the right of septum primum blood glucose meter japan generic amaryl 3mg line, the leading margins of septum secundum constitutes what is called the superior limbus of fossa ovalis diabetes symptoms 10 year old discount 4mg amaryl visa. They found that spontaneous closure occurred in 22 percent in patients who had their cardiac catheterization before the first year of life blood sugar two hours after eating generic 3mg amaryl with visa. This decreased to 3 percent in patients who were between 2 to 4 years at the time of their 1st cardiac catheterization diabetes mellitus medscape cheap amaryl 4mg. In 65 percent of patients the defects enlarged, some to the extent that they could not be closed by transcatheter techniques at that time. In summary, defects larger than 8 to 10 mm are less likely to close spontaneously and most likely will require surgical or transcatheter closure, regardless of the age at diagnosis. We will discuss below possible the complications that can ensue from interatrial communications. It is still debatable whether this is caused by the presence of large shunts or due to other predisposing conditions such as thromboembolic phenomena. This was confirmed by comparative studies that found existing risk even in patients who do not have atrial arrhythmias. Reduced Life Expectancy Secondary to pulmonary arterial thrombosis, congestive heart failure, paradoxical embolism and recurrent respiratory infections. This explains the timing of presentation for large shunts in infancy, which usually occurs between 6 to 8 weeks. At that point, the pulmonary vascular resistance drops to its normal levels and the right ventricle becomes more compliant, leading to increase pressure gradient between the two atria and subsequently a larger shunting volume. This is rarely the case in children, where congestive heart failure or failure to thrive are very uncommon. Most of the time physical examination is unremarkable, typical physical findings include normal oxygen saturation, apart from aforementioned conditions. Other findings include wide fixed splitting of the second heart sound, which is an exaggeration of a normal phenomena that leads to delay in closure of the pulmonary valve as a reflection of the dilation of the pulmonary artery that warrants longer time to achieve adequate pressure to close the pulmonary valve, other factors that explain this, is the prolonged emptying of the right ventricle. Auscultatory findings also include soft crescendodecrescendo ejection systolic murmur on the left upper sternal border as a result of pulmonary blood overflow across that valve and a mid-diastolic murmur at the lower left sternal border related to increased blood flow across the tricuspid valve in larger shunts. Once pulmonary hypertension develops these findings completely change to a cyanotic patient with prominent second heart sound, short systolic murmur and absent fixed splitting or diastolic murmur. Enlarged cardiac silhouette can also be seen as a consequence of prolonged volume overload to the right atrium and ventricle. In fact, most children present with a murmur on incidental cardiac examination or when they are referred for cardiology consultation for other purposes. Findings are 255 4 Shunt DefectS this indeed is not seen in case of pulmonary obstructive disease; on the contrary, the lung fields at that point would be oligemic. In most instances the rhythm is normal sinus, but sometimes and especially at an older age there might be evidence of atrial fibrillation or atrial flutter. This is achieved by finding the best view where the echo beam is perpendicular to the defect. However, it is appropriate for evaluation of right ventricular dilation and estimation of right ventricular systolic pressure using tricuspid regurgitation jet. Parasternal short-axis view might offer an alternative for the subcostal view in the adult population, high right parasternal view in right decubitus position is particularly useful. Coronary sinus defects should be suspected when a dilated coronary sinus is seen with dilated right atrium and right ventricle. Four-chamber apical view: this demonstrates the atrial septal defect (arrow) and dilated right atrium and right ventricle; B. Parasternal short-axis view showing the defect (arrow) and the deficient anterior (aortic rim) and the posterior rim confirmed shunt on color Doppler; E and F. Subcostal sagittal view of showing the defect (arrow) and superior inferior margins with left-to-right shunt. Looking carefully in subcostal sagittal view a sinus venosus defect is appreciated. In this particular case, the coronary sinus is completely unroofed in what is called Raghib syndrome. Contrast Echocardiography Verification of the presence of interatrial communication can sometimes be challenging, particularly if the defect is small or the acoustic windows are not optimal in older adults. Peripheral intravenous line can be used to inject agitated saline using a three-way stopcock, while imaging the atria in 4-apical view. Air bubbles should opacify the right atrium, negative wash out will be seen in the case of left-to-right shunt. This technique is used more frequently to look for presence of right-to-left shunt at rest or during Valsalva maneuver. They provide wide field view with detailed resolution of the defect and the adjacent structures, specifically the pulmonary veins without the limitation of poor acoustic windows sometimes encountered in echocardiography. Transesophageal 2D Echocardiography Transesophageal echocardiogram, is used in adult patients whom the transthoracic acoustic windows are not optimal. Color Doppler also confirms presence of left-to-right shunt as seen by the blue jet; C and D. Color Doppler is seen in D showing left- to-right shunt across the defect; E and F. Other indications include partial anomalous pulmonary venous return where non-invasive data are nonconclusive for the course of these veins and their drainage. Otherwise, hemodynamic study is performed as part of an interventional procedure during device closure of these defects. As it is the case in most congenital heart diseases, presence of symptoms is certainly an indication for closure. The 4 chamber view is a superoposterior and inferoanterior cut into the defect and this shows the relationship to the atrioventricular valves. Right ventricular volume overload is not expected as a hemodynamic consequence of such defects. Follow-up of such patients who do not meet the criteria for closure includes an echocardiogram every 2 to 3 years looking for development of any criteria warranting closure. Patients with larger defects will suffer ultimately from complications later in their lives. For that reason, patients who present with large defects (> 8 mm), large shunts (Qp: Qs more than 1. Clinical and laboratory findings of right ventricular volume overload can manifest with physical findings of diastolic flow rumble due to tricuspid regurgitation, cardiomegaly and increase pulmonary vascular markings on chest X-ray, signsof right ventricular hypertrophy on electrocardiograms and ultimately echocardiographic findings of right ventricular hypertrophy with possible paradoxical wall motion of the ventricular septum. Development of inevitable sequelae of large shunts later in life further complicates the management of older patients. This, however, should be preceded by successful cardioversion or ablation before the access to left atrium is closed. Careful evaluation of these patients should include cardiac catheterization to determine the operability and risk of closure. It allows direct measurement of the pulmonary arterial pressure and pulmonary vasoreactivity test with oxygen or nitric oxide. Balloon occlusion testing temporarily in the cardiac catheterization laboratory can provide insight to the risk of closure in patients with reversible pulmonary hypertension or bidirectional shunt or in patients whose response to medical therapy for pulmonary hypertension is evaluated prior to closure of the defect. Several studies tried to identify patients at high risk of mortality and morbidity for shunt closure. First: elderly patients who develop left ventricular diastolic dysfunction as a result of ischemic heart disease, hypertension or acquired valvular disease are considered a high risk for closure. Elevated left ventricular end-diastolic pressure reflected by high pulmonary wedge pressures should be anticipated. Adequate medical treatment prior to closure of the defect and balloon test occlusion before closing the defect are advised. In this condition, despite the finding of cyanosis, closure of the defect is considered curative. Associated anomalies should be identified prior to surgery: cleft in the mitral valve in septum primum defects should be repaired at the same time, while in sinus venosus defects, identification of right upper/middle pulmonary venous drainage should be taken into consideration during surgery. Minimally invasive surgeries nowadays avoid midsternotomy approach using different less extensive incisions for cosmetic purposes. One of the major findings was the excellent outcome and low operative mortality especially at a younger age ranging between 0 to 1 percent. Long-term survival after surgical closure in childhood showed that no change from the general population. Murphy et al31 in a follow-up study of patients operated between 1956 to 1960 showed that survival among patients younger than 24 years were no different from rates among controls. Patients over 41 years of age, on the other hand, survival rates were significantly less. Independent predictors of long-term survival according to multivariate analysis were age at operation and systolic pressure in the main pulmonary artery before operation. Late heart failure, stroke and atrial fibrillation were significantly more frequent in older patients thus requiring close follow-up. In fact, Berger et al19 showed atrial arrhythmias persisted in more than 48 percent after surgery in patients older than 60 years which did not show significant improvement from incidence prior to surgery. They concluded that in this group of high-risk patients (with atrial fibrillation) surgical atrial closure should be combined with Cox-maze procedure. Pulmonary vascular disease had been proven to be a strong predictor of poor outcome after surgery. Regression in symptoms and lower mortality rate were noticed postoperatively in this group although they usually have an expected difficult immediate postoperative course. It was not until 2002 when the non-randomized multicenter study that compared percutaneous approach using Amplatzer device in more than 400 patients to surgical approach was reported. It demonstrated similar success rates, lower complication rate and shorter hospital stay in the device closure group versus the surgical repair group. Nevertheless, there are defects that are nonamenable to this approach in which surgery should be the appropriate option for closure. Secundum atrial defects that are larger than 38 mm in diameter or defects that have insufficient rims (< 5 mm) are also not suitable for transcatheter device closure. High-risk patients include extremes of age: infants due to the need of large sheath size and risk of vessel injury and elderly patients with left ventricular dysfunction. Other relative contraindications include active infection, pregnancy, uncontrolled arrhythmias or conditions where antiplatelet therapy is not tolerated. A recent long-term follow-up study showed an incidence of 7 percent of documented arrhythmias in patients who received the Amplatzer septal occluder between 1998 to 2002. Such arrhythmias included mainly supraventricular tachycardia, atrial fibrillation and premature ventricular beats. Although current devices are less thrombogenic, antiplatelet therapy with clopidogrel and Aspirin are used for 2 to 12 months. Post-procedure atrial fibrillation and persistent atrial septal aneurysm had been found as significant predictors for thrombus formation. The safe and effective nonsurgical option to close interatrial defects should be assured by proper patient selection, continuous assessment during device closure and close monitoring after deployment of the appropriate device. Although usually carries benign course in childhood, it has significant morbidity with advancing age. Safe non-surgical option via transcatheter closure is available for certain types of defects. Deployment of the device under continuous echocardiographic guidance after selecting the appropriate type and size of the device. Incidence and size of patent foramen ovale during the first 10 decades of life: An autopsy study of 965 normal hearts. Embryology of the atrioventricular canal region and pathogenesis of endocardial cushion defects. Reduced penetrance, variable expressivity, and genetic heterogeneity of familial atrial septal defects. Spontaneous closure of secundum atrial septal defect in infants and young children. Predictive factors for spontaneous closure of atrial septal defects diagnosed in the first 3 months of life. Predictors of spontaneous closure of isolated secundum atrial septal defect in children: a longitudinal study. Natural history of growth of secundum atrial septal defects and implications for transcatheter closure. Incidence of atrial flutter/ fibrillation in adults with atrial septal defect before and after surgery. Isolated atrial septal defect with pulmonary vascular obstructive disease: Long-term follow-up and prediction of outcome after surgical correction. A report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Guidelines for evaluation and management of common congenital cardiac problems in infants, children, and adolescents. A statement for healthcare professionals from the Committee on Congenital Cardiac Defects of the Council on Cardiovascular Disease in the Young. Development of a Pump-oxygenator to Replace the Heart and Lungs: An Apparatus Applicable to Human Patients and Application to One Case Ann Surg. Surgical closure of atrial septal defects in adults: effect of age at operation on outcome. Sinus venosus atrial septal defect: long-term postoperative outcome for 115 patients. Long-term follow up of secundum atrial septal defect closure with the Amplatzer septal occluder. Incidence and clinical course of thrombus formation on atrial septal defect and patient foramen ovale closure devices in 1,000 consecutive patients. It is revealed only by auscultation and shows itself by a physical sign with quite distinctive characteristics: this is a loud, prolonged whirring sound; it is a single murmur, beginning with systole and continuing in such a way as to entirely mask the normal rhythm; its maximum intensity is not at the apex or at the right or left side of the base, but over the upper third of the precordial region; it is central like the septum itself and diminishes gradually from this central point the farther from it one listens; it is not transmitted; it corresponds to no other sign of organic disease except the purring thrill.
Cheap amaryl online amex. How to cure diabetes permanently naturally.


















