Procardia

James B. Seward, MD, FACC
- Professor of Medicine and Pediatrics
- Division of Cardiovascular Research
- Mayo Clinic Rochester
- Rochester, Minnesota
Endoscopic third ventriculostomy with cystoventricular stent placement in the management of DandyWalker malformation: technical case report of three patients coronary heart ratio discount procardia 30 mg overnight delivery. The roof and lateral recesses of the fourth ventricle considered morphologically and embryologically heart disease for women generic procardia 30mg amex. Cerebellum-small brain but large confusion: a review of selected cerebellar malformations and disruptions coronary heart disease journal pdf buy procardia once a day. A syndrome of episodic hyperpnea cardiovascular system penyakit jantung koroner cheap 30mg procardia amex, abnormal eye movements cardiovascular workout crossword generic procardia 30 mg fast delivery, ataxia arteries ks2 order procardia 30mg mastercard, and retardation. Joubert syndrome: a model for untangling recessive disorders with extreme genetic heterogeneity. Defective Wnt-dependent cerebellar midline fusion in a mouse model of Joubert syndrome. Primary cilia are required for cerebellar development and Shh-dependent expansion of progenitor pool. Rhombencephalosynapsis associated with cutaneous pretibial hemangloma in an infant. Prenatal magnetic resonance imaging of rhombencephalosynapsis and associated brain anomalies-report of 3 cases. Human malformations of the midbrain and hindbrain: review and proposed classification scheme. Pontocerebellar hypoplasia: review of classification and genetics, and exclusion of several genes known to be important for cerebellar development. Frequency and nature of cerebellar injury in the extremely premature survivor with cerebral palsy. Injury of the developing cerebellum: a brief review of the effects of endotoxin and asphyxial challenges in the late gestation sheep fetus. Cerebellar growth and behavioural and neuropsychological outcome in preterm adolescents. Injury to the premature cerebellum: outcome is related to remote cortical development. Current perspectives on the role of thyroid hormone in growth and development of cerebellum. Thyroid hormone role on cerebellar development and maintenance: a perspective based on transgenic mouse models. Early maternal hypothyroxinemia alters histogenesis and cerebral cortex cytoarchitecture of the progeny. Neonatal outcomes and birth weight in pregnancies complicated by maternal thyroid disease. Role of late maternal thyroid hormones in cerebral cortex development: an experimental model for human prematurity. The effects of early hypo- and hyperthyroidism on the development of rat cerebellar cortex. The effects of early hypo- and hyperthyroidism on the development of the rat cerebellar cortex. Some mechanisms of cerebellar foliation: effects of early hypo- and hyperthyroidism. Effects of thyroid hormone on synaptogenesis in the molecular layer of the developing rat cerebellum. Failure of thyroid hormone treatment to prevent inflammation-induced white matter injury in the immature brain. Neurosteroids in the brain neuron: biosynthesis, action and medicinal impact on neurodegenerative disease. Steroid synthesis and metabolism in the nervous system: trophic and protective effects. Inhibition of neurosteroid synthesis increases asphyxia-induced brain injury in the late gestation fetal sheep. Elevated levels of umbilical cord plasma corticotropin-releasing hormone in growth-retarded fetuses. Glucocorticoids, feto-placental 11 beta-hydroxysteroid dehydrogenase type 2, and the early life origins of adult disease. Neonatal pain and infection relate to smaller cerebellum in very preterm children at school age. Internalizing behaviours in school-age children born very preterm are predicted by neonatal pain and morphine exposure. Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Neonatal pain-related stress predicts cortical thickness at age 7 years in children born very preterm. Three-dimensional distribution of 3H-naloxone binding to opiate receptors in the human fetal and infant brainstem. Opioid receptors localize to the external granular cell layer of the developing human cerebellum. Morphine inhibits Purkinje cell survival and dendritic differentiation in organotypic cultures of the mouse cerebellum. Association between preterm brain injury and exposure to chorioamnionitis during fetal life. The impact of prenatal and neonatal infection on neurodevelopmental outcomes in very preterm infants. Initially, a tangential stream of migration from the ganglionic eminence leads to the formation of the marginal zone, or preplate. All radially migrating neurons and glia are derived from the ventricular and subventricular zones, present in the subependymal location at every level of the developing nervous system. These events span a period from the second month of gestation to adult life, including the perinatal period. Aberrations of brain development may be an important consequence of genetic perturbations as well as a variety of prenatal and perinatal insults at critical times during development. This article reviews the normal aspects of neuronal proliferation and discusses disorders encountered when normal development goes awry. When cells withdraw from the mitotic cycle and cease proliferative activity, they migrate into the intermediate zone on their way to forming the cortical plate (see later discussion). The elegant work of Caviness and coworkers defined the G1 phase of the cell cycle as the molecular control point for these critical proliferative events. Later, at a time comparable to the second half of the second month of gestation in the human, the number of these proliferative units becomes stable as the progenitor cells begin to divide asymmetrically. Proliferative units later enlarge by asymmetrical divisions of progenitor cells before neuronal migration. These asymmetrical divisions determine the size of each proliferative unit (see Box 5. As the proliferative phase progresses, proportionately more postmitotic neuronal cells and fewer stem cells are produced. Rakic showed that the distinguishing features of the kinetics of neuronal proliferation in primates versus species with smaller neocortices are a longer cell cycle duration and, particularly, a more prolonged developmental period of neuronal proliferation. Thus the term radial glial cell (which we continue to use) may ultimately be replaced by radial glial progenitor or radial progenitor. These elegant proliferative events involving the radial glial cell as neuronal progenitor are modulated by several key signaling pathways involving the Notch receptor, the ErbB receptor (through the ligand neuregulin), and the fibroblast growth factor receptor. Subsequent to neurogenesis, radial cells produce astrocytes and other glial cells. The classical understanding of neuronal proliferation and migration centers on the ventricular and subventricular zones and radially migrating neurons. The dural venous sinuses, the arachnoidal arterial and venous systems, and the pial plexus that characterize the adult brain are already recognizable at this age. The wall of the cerebral cortex (cerebral vesicle) has been opened to demonstrate that, at this age, its intrinsic vascularization has not started, but that of the choroid plexus is already under way. Because of difficulties in quantitating neuronal populations, however, proliferative disorders are often difficult to define by conventional neuropathological examination. Even when the disorder is so extreme that the brain is grossly undersized (as in microcephaly) or oversized (as in macrocephaly), defining the nature and severity of the proliferative derangement is also difficult by conventional techniques. Microcephaly means "small head," as opposed to micrencephaly, which means "small brain. Barring severe cranial defects resulting in premature skull closure, small brain size is generally considered the reason for small head size. We distinguish primary microcephalies, apparently related to impaired neuronal proliferation resulting in too few neurons, from microcephalies secondary to destructive disease (Box 5. Microcephaly vera refers to a heterogeneous group of disorders that appear to have, as the common denominator, small brain size because of a derangement of proliferation (see Box 5. The brain is generally well formed, although the gyrification pattern may be simplified to a variable degree, sometimes but not always commensurate with the degree of microcephaly. We first discuss radial microbrain, an informative but rare and particularly severe type of microcephaly vera, and then the more common genetically determined varieties of microcephaly vera. Radial microbrain is a rare disorder of particular interest because it appears to provide the first clear example of a disturbance in the number of proliferative units resulting in small brain size. The extremely small brain has no marked gyral abnormality, no evidence of a destructive process, and no disturbance of cortical lamination. The conclusion that the disturbance involves the early phase of proliferative events, by which symmetrical divisions of neuronal progenitors generate the total number of proliferative units, is based on the finding of a marked reduction in number of cortical neuronal columns but an apparent normal complement of the neurons per column. The presumed timing of radial microbrain is no later than the earliest phase of proliferative events in the second month of gestation. The essential abnormality involves the symmetrical divisions of progenitors to form additional progenitors and thereby the ks re ks fre fre ks f ks fre. The reported cases have involved full-term newborns who died in the first month of life. The distinction from anencephaly and aprosencephaly-atelencephaly is based on the presence of an intact skull and dermal covering, in contrast to anencephaly, and of a normal external appearance of cerebrum and ventricles, observable by ultrasonography, in contrast to aprosencephaly-atelencephaly. Although the cerebral surface in primates expands and shifts during prenatal development, ontogenetic columns (outlined by cylinders) may remain attached to the corresponding proliferative units by the grid of radial glial fibers. As a result, proliferative units 1 to 100 produce ontogenetic columns 1 to 100 in the same relative position to each other without a lateral mismatch. Thus the specification of cytoarchitectonic areas and topographic maps depends on the spatial distribution of their ancestors in the proliferative units, whereas the laminar position and phenotype of neurons within ontogenetic columns depend on the time of their origin. In A, as occurs especially early in neuronal proliferation, a single neural precursor gives rise to two identical precursors, that is, a symmetrical division. In B as occurs especially later in neuronal proliferation, a radial neuronal progenitor (radial glial progenitor or radial glial cell) divides asymmetrically into dissimilar cells, that is, an identical radial progenitor and a postmitotic neuronal cell that migrates along the fiber of its clonally related radial progenitor to ultimately reach the cerebral cortex. As noted earlier, the designation microcephaly vera refers to a heterogeneous group of autosomal recessive disorders that appear to have, as the common denominator, small brain size because of a derangement of proliferation (see Box 5. In recent years, remarkable insights into the genetics and molecular bases of these disorders have been gained (see later). Brain of a full-term newborn with the pathological picture of radial microbrain described in the text. Note the normal cortical lamination (long arrows) and the normal residual germinative zone (both open arrows). Simplification of gyral pattern exists with no other external abnormality and no evidence of a destructive process. The number of cortical neuronal columns appears normal, but the neuronal complement of each column, especially the superficial cortical layers, is decreased markedly. Additional evidence of disturbance of the later proliferative events that determine size of cortical neuronal columns is the absence of residual germinal matrix in the 26-week fetal brain studied by Evrard et al. The deficiency in neurons of the superficial cortical layers may explain the simplification of gyral pattern (see the later discussion of gyral development in migrational disorders in Chapters 6 and 7). The presumed timing of the microcephaly vera group of disorders involves the period of later proliferative events by asymmetrical divisions of neuronal progenitors-that is, onset at approximately 6 weeks in the human-with later rapid progression until approximately 18 weeks (see earlier). The most severely undersized brains are expected to have the earliest onsets and the most marked deficiency of neurons in each cortical column. Rare autosomal recessive forms of microcephaly with severe neuronal migrational defects. Rare cases are associated with severe migrational disturbances, such as lissencephaly, periventricular heterotopia, or posterior fossa deficits, especially cerebellar hypoplasia. The germinal layer (arrowheads), cerebral cortex (arrows), and intervening cerebral white matter are visible. In microcephaly vera (A), the germinal layer is exhausted at this age, and the white matter is almost devoid of late migrating glial and neuronal cells. No other dysgenetic abnormalities are present, nor is there any evidence of destructive disease. Genes have been identified for the majority of the loci, though sometimes only in one family (Table 5. The four major etiological categories for primary microcephaly, in addition to the autosomal recessive group just discussed, are familial, teratogenic, syndromic, and sporadic (see Box 5. Familial syndromes are most critical to detect because of implications for genetic counseling. At least to the autosomal recessive group (see earlier), these inherited varieties include autosomal dominant and X-linked recessive types as well as familial types with ocular abnormalities and variable genetics. One such disorder is Cohen syndrome, which is inherited in an autosomal recessive manner. Of the unusual cases of microcephaly with autosomal dominant inheritance, intellect is subsequently usually either spared or only mildly defective; patients generally have no facial dysmorphism, although digital anomalies and rare syndromic varieties have been reported. The best-documented teratogenic agent producing microcephaly is irradiation, such as that due to an atomic explosion or radiation therapy for tumor or ankylosing spondylitis, particularly before 18 weeks of gestation (see Box 5.
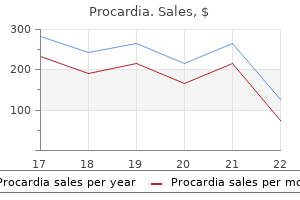
Preliminary data suggest superiority of cyanoacrylate obturation of gastric varices over -blockers to prevent the first gastric variceal bleed coronary heart leaf order procardia online from canada. When a patient is diagnosed to have acutely bleeding gastric varices on endoscopy blood vessels histology slides purchase discount procardia line, obturation of the varices with cyanoacrylate glue is the treatment of choice cardiovascular x-ray order 30mg procardia amex. Initial management and resuscitation of these patients is no different than in patients with esophageal variceal hemorrhage cardiovascular system labeling worksheet generic 30 mg procardia amex. A cardiovascular disease effects 30 mg procardia with visa,Activelybleeding (pentagon) gastric varix (black arrow) with large amount of blood (arrowhead) pooling in stomach capillaries rash on legs cheap 30 mg procardia overnight delivery. Standard sclerosing agents are not effective in the control of gastric variceal bleeding and are associated with a high risk of rebleeding. In a randomized controlled trial, initial hemostasis up to 72 hours was achieved in 87% of patients treated with cyanoacrylate obturation but in only 45% of patients who were banded. Acute bleeding is treated with vasoactive agents similar to patients with esophageal variceal bleeding. To prevent rebleeding in patients with iron deficiency anemia, nonselective -blockers are used, usually in combination with iron replacement. Ectopic Varices Manifestations of ectopic variceal bleeding include hematemesis or melena, but hemobilia, hematuria, and intraperitoneal or retroperitoneal bleeding also occur. Patients with extrahepatic vein obstruction usually bleed from varices at the gastroesophageal junction, or in the duodenum. Patients with cirrhosis, on the other hand, tend to bleed from sites where surgery has allowed the development of ectopic varices, usually peristomal varices. Initial control of stomal variceal bleeding is local compression of the bleeding site with gauze soaked with a 1: 10,000 epinephrine solution. It is important to note that selective shunts, such as the distal splenorenal shunt, are ineffective in preventing bleeding from stomal varices. Bleeding from ectopic varices, other than stomal varices, is initially treated much the same way as varices at other sites. Endoscopic therapy includes band ligation, glue injection, and application of clips. In addition, surgical ligation may need to be considered for refractory bleeding varices, especially when associated with intraabdominal hemorrhage. Additionally innovations in endoscopic and radiographic procedures along with clinical studies comparing treatment options also drive progress. These advances are exemplified by reductions in mortality associated with portal hypertensive bleeding. However, many gaps remain before treatment of portal hypertension and its associated bleeding are optimized. Iwakiri Y, Grisham M, Shah V: Vascular biology and pathobiology of the liver: report of a single-topic symposium. Bhathal P, Grossman H: Reduction of the increased portal vascular resistance of the isolated perfused cirrhotic rat liver by vasodilators. Bhathal P, Grossman H: Active contractile and mechanical factors in the pathogenesis of portal hypertension-a study utilizing three experimental models. Shah V, et al: Liver sinusoidal endothelial cells are responsible for nitric oxide modulation of hepatic resistance. Omenetti A, et al: Hedgehog signaling regulates epithelialmesenchymal transition during biliary fibrosis in rodents and humans. Zipprich A, et al: Nitric oxide and vascular remodeling modulate hepatic arterial vascular resistance in the isolated perfused cirrhotic rat liver. Patsenker E, et al: Pharmacological inhibition of integrin alphavbeta3 aggravates experimental liver fibrosis and suppresses hepatic angiogenesis. Semela D, et al: Platelet-derived growth factor signaling through ephrin-B2 regulates hepatic vascular structure and function. Tugues S, et al: Antiangiogenic treatment with sunitinib ameliorates inflammatory infiltrate, fibrosis, and portal pressure in cirrhotic rats. Novo E, et al: Proangiogenic cytokines as hypoxia-dependent factors stimulating migration of human hepatic stellate cells. Iwakiri Y: the molecules: mechanisms of arterial vasodilatation observed in the splanchnic and systemic circulation in portal hypertension. Fernandez M, et al: Reversal of portal hypertension and hyperdynamic splanchnic circulation by combined vascular endothelial growth factor and platelet-derived growth factor blockade in rats. Schepis F, et al: Which patients with cirrhosis should undergo endoscopic screening for esophageal varices detection Escorsell A, et al: Increasing intra-abdominal pressure increases pressure, volume, and wall tension in esophageal varices. Procopet B, et al: Real-time shear-wave elastography: applicability, reliability and accuracy for clinically significant portal hypertension. La Mura V, et al: Right atrial pressure is not adequate to calculate portal pressure gradient in cirrhosis: a clinical-hemodynamic correlation study. Summary of an American Association for the study of liver diseases and European Association for the study of the liver single-topic conference. Escorsell A, et al: Predictive value of the variceal pressure response to continued pharmacological therapy in patients with cirrhosis and portal hypertension. Levesque E, et al: Plasma disappearance rate of indocyanine green: a tool to evaluate early graft outcome after liver transplantation. Siramolpiwat S, et al: Idiopathic portal hypertension: natural history and long-term outcome. Boyer T, et al: Direct transheaptic measurement of portal vein pressure using a thin needle. Singh S, et al: Identifying the presence of clinically significant hepatic involvement in hereditary haemorrhagic telangiectasia using a simple clinical scoring index. Berzigotti A, et al: Elastography, spleen size, and platelet count identify portal hypertension in patients with compensated cirrhosis. Thabut D, Moreau R, Lebrec D: Noninvasive assessment of portal hypertension in patients with cirrhosis. Berzigotti A, et al: Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Bambha K, et al: Predictors of early re-bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis. Kamath P, et al: Gastric mucosal responses to intrahepatic portosystemic shunting in patients with cirrhosis. Primignani M, et al: Natural history of portal hypertensive gastropathy in patients with liver cirrhosis. Cales P, et al: Early administration of vapreotide for variceal bleeding in patients with cirrhosis. Villanueva C, et al: Acute hemodynamic response to beta-blockers and prediction of long-term outcome in primary prophylaxis of variceal bleeding. Tripathi D, et al: Randomized controlled trial of carvedilol versus variceal band ligation for the prevention of the first variceal bleed. Bosch J, Garcia-Tsao G: Pharmacological versus endoscopic therapy in the prevention of variceal hemorrhage: and the winner is. Mahadeva S, et al: Cost-effectiveness of N-butyl-2-cyanoacrylate (histoacryl) glue injections versus transjugular intrahepatic portosystemic shunt in the management of acute gastric variceal bleeding. Malinchoc M, et al: A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Cardenas A, Fernandez-Simon A, Escorcell A: Endoscopic band ligation and esophageal stents for acute variceal bleeding. Cales P, et al: Lack of effect of propranolol in the prevention of large oesophageal varices in patients with cirrhosis: a randomized trial. Merkel C, et al: A placebo-controlled clinical trial of nadolol in the prophylaxis of growth of small esophageal varices in cirrhosis. Bernard B, et al: Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Fernandez J, et al: Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Ripoll C, et al: Rebleeding prophylaxis improves outcomes in patients with hepatocellular carcinoma. Bernard B, et al: Beta-adrenergic antagonists in the prevention of gastrointestinal rebleeding in patients with cirrhosis: a metaanalysis. Villanueva C, et al: Nadolol plus isosorbide mononitrate compared with sclerotherapy for the prevention of variceal rebleeding. Gonzalez R, et al: Meta-analysis: Combination endoscopic and drug therapy to prevent variceal rebleeding in cirrhosis. Cho S, et al: Endoscopic cryotherapy for the management of gastric antral vascular ectasia. Likewise, patients with underlying chronic renal damage may develop superimposed hemodynamic compromise, adding a functional component to worsening renal failure. Hepatologists are now borrowing various classifications from other subspecialties and modifying them for cirrhotic patients so that we can define these cases of acute renal failure more appropriately. This article will firstly concentrate on acute functional renal failure, especially with respect to its changing definition in cirrhosis. Measurement of Renal Function Renal function is traditionally evaluated by measurement of the serum creatinine concentration as it is cheap and readily available. The serum creatinine is usually filtered by the glomeruli and then not reabsorbed by the renal tubule, so whatever creatinine appears in the urine represents what is being filtered. However, both serum creatinine and creatinine clearance measurements are steady-state measurements, and these can become less precise in the setting of acute renal failure. In the case of patients with advanced cirrhosis, the production of creatinine from creatine is reduced because of significant muscle wasting in these patients, adding to the inaccuracy in the use of serum creatinine concentration as a measure of renal function. It is estimated that 20% of cirrhotic patients admitted to hospital have some form of renal dysfunction, most cases of which are related to acute renal failure, whereas chronic renal failure constitutes only 1% of cases. The most interesting observation was that even trivial changes in renal function could be Acute Kidney Injury Functional Renal Failure Structural renal disease. This came about because it was noted that in patients who had undergone cardiovascular surgery, even a small increase of serum creatinine concentration of 0. However, renal replacement therapy has been added as a diagnostic criterion for the severest stage. Renal replacement therapy was not included as part of the staging, as it was felt that it more appropriately described patient outcome rather than the severity of kidney dysfunction. Acute-on-chronic kidney disease Rise in serum creatinine concentration of 50% from the baseline or a rise of serum creatinine concentration of 0. For the first time the term acute kidney injury was formally adopted to represent acute renal failure in cirrhosis. The groups felt that serum creatinine concentration, despite its many shortcomings,15,16 should be maintained as a measure of renal function, because of its simplicity of use and the wide availability of the test. However, the groups spent quite some time debating the definition of the baseline serum creatinine concentration, especially in patients who did not have regular measurements of serum creatinine. The groups also decided to discard the urine output diagnostic criterion, as oliguria is a cardinal feature of cirrhosis with ascites. Working party proposal for a revised classification system of renal dysfunction in patients with cirrhosis. In any event, comparison was confounded by the fact that the two groups were not equal at baseline. A stable outpatient serum creatinine concentration closest to the index admission value was used as the baseline value. In situations where there was no outpatient serum creatinine concentration available, the serum creatinine that had been stable for 5 days after admission was used as the baseline. Despite this, the development of mild renal dysfunction had a negative effect on patient survival. Despite this, there was a significant and gradual rise in the serum creatinine concentration associated with reduced survival when patients were followed up for 12 months. This highlights the fact that even minor changes in renal function influence the course of decompensated cirrhosis. It is clear from the foregoing discussion that the various diagnostic criteria have some utility in predicting patient outcomes in the cirrhotic population. This is incongruent with the thought process of the nephrology and intensive care specialties, which firmly believe that a reduced urine output is the first sign suggesting the development of renal dysfunction, even before any change in serum creatinine concentration is noted. Some studies also used the most recent serum creatinine measurement before hospital admission as the baseline serum creatinine. In a recent study including 213 patients hospitalized for acute decompensation of cirrhosis with an admission serum creatinine of less than 1. Furthermore, such a derived serum creatinine value was not able to predict 90-day survival. With all the ongoing issues relating to these various diagnostic criteria, many feel that they create more confusion than help in the care of cirrhotic patients, especially because none of the studies mentioned above provided any guidelines on the treatment of patients with cirrhosis and renal failure. Therefore not all members of the hepatology community have favored the change from the traditional diagnostic criteria for renal failure in cirrhosis,29,30 which requires a 50% increase in serum creatinine with the final serum creatinine concentration reaching 1. This is especially true because this traditional definition of renal failure in cirrhosis has accurately predicted patient outcome in cirrhosis. Further studies will undoubtedly lead to further refinements of how we will describe renal failure in cirrhosis in the future. Clinicians also have problems in making treatment decisions for cirrhotic patients with renal dysfunction, especially regarding the use of vasoconstrictor therapy. There was also consensus that serum creatinine concentration should be used as the index of renal function despite all its limitations. This is because clinicians are familiar with its use and the test is widely available.
Buy procardia 30 mg cheap. #IDoR2018 #Cardiac Basics of #Coronary #Anatomy.
Any bilomas that have resulted from the bile leak should be managed with drainage coronary artery nomenclature discount procardia 30 mg mastercard. A transhepatic wire is placed into the biliary tree under fluoroscopic guidance across the stricture coronary heart disease journal order procardia overnight delivery, with contrast opacification of the jejunum confirming passage across the anastomotic stricture (A) capillaries refill purchase procardia 30mg amex. Healing of a nonoperatively managed biliary fistula may result in late stricture formation and thus may necessitate future surgical biliary revision heart disease myths order generic procardia. Biliary strictures account for two thirds of biliary complications after liver transplantation cardiovascular system yoga order procardia with paypal,140 often presenting with elevated liver tests and/or abdominal pain cardiovascular institute of orlando purchase genuine procardia on line. Biliary obstruction with ascending cholangitis or intrahepatic abscess formation remains a serious complication. Whereas early anastomotic stricture is usually related to errors in the surgical technique, late biliary stricture formation is often at the level of the anastomosis, and secondary to ischemia. Ultrasound examination in liver transplant recipients has a low sensitivity (50%) in establishing a diagnosis of biliary stricture given the frequent lack of ductal dilatation. The endoscopic approach has yielded success rates of 62% for deceased donor recipients, and 75% for living donor recipients. Rare but serious complications associated with the transhepatic route include hemobilia, hepatic artery pseudoaneurysm formation, arterioportal fistula creation, and portal vein thrombosis. Operative intervention entails surgical excision of the stricture, with conversion of the choledochocholedochotomy to a choledochojejunostomy. Although anastomotic strictures are the most frequent type of biliary stricture in the liver transplant recipient, diffuse intrahepatic strictures are far more problematic. Generalized ischemia of the entire biliary tree is believed to be the etiologic agent leading to diffuse stricture disease. Diffuse intrahepatic strictures are associated with microscopic or macroscopic abscesses and commonly recurrent biliary sepsis. Deceased donor liver transplantation is associated with a 15% to 25% biliary stricture rate146 whereas living donor liver transplantation has a significantly higher incidence of biliary complications (30%). Retrospective reviews have demonstrated a lower stricture rate in patients undergoing choledochojejunostomy (8. However, the duct-to-duct anastomosis was shown to have a significantly lower incidence of leakage (4. In addition, 1767 patients died waiting for a liver transplant, with an additional 1223 removed from the waitlist due to being too sick to undergo transplant. Conclusion With advances in surgical technique, immunosuppression, and critical care, liver transplantation has become the management of choice for patients with acute and chronic liver failure, metabolic diseases with their primary defect residing in the liver, and unresectable primary liver tumors without evidence of extrahepatic spread. Advances in immunosuppression regimens have improved both graft and patient survival. However, side effects associated with chronic immunosuppression continue to cause substantial long-term morbidity and mortality. Indeed, it is the shortage of donor organs and the need for chronic immunosuppression which represent the remaining formidable obstacles to the greater application and durable success of liver transplantation. Kalayoglu M, et al: Extended preservation of the liver for clinical transplantation. Mazzaferro V, et al: Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. Goldberg D, et al: Increasing disparity in waitlist mortality rates with increased model for end-stage liver disease scores for candidates with hepatocellular carcinoma versus candidates without hepatocellular carcinoma. Mehta N, et al: Identification of liver transplant candidates with hepatocellular carcinoma and a very low dropout risk: implications for the current organ allocation policy. Hameed B, et al: Alpha-fetoprotein level > 1000 ng/mL as an exclusion criterion for liver transplantation in patients with hepatocellular carcinoma meeting the Milan criteria. Schlansky B, et al: Waiting time predicts survival after liver transplantation for hepatocellular carcinoma:a cohort study in the unos registry. Bharat A, et al: Pre-liver transplantation locoregional adjuvant therapy for hepatocellular carcinoma as a strategy to improve longterm survival. Cescon M, et al: Hepatocellular carcinoma locoregional therapies for patients in the waiting list. Report of the ad hoc committee of the Harvard Medical School to examine the definition of brain death. Feng S, et al: Characteristics associated with liver graft failure: the concept of a donor risk index. Bismuth H, Houssin D: Reduced-sized orthotopic liver graft in hepatic transplantation in children. Pichlmayr R, et al: Transplantation of a donor liver to 2 recipients (splitting transplantation)-a new method in the further development of segmental liver transplantation. Reyes J, et al: Split-liver transplantation: a comparison of ex vivo and in situ techniques. Yamaoka Y, et al: Liver transplantation using a right lobe graft from a living related donor. Dahm F, et al: Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Ikegami T, et al: Current concept of small-for-size grafts in living donor liver transplantation. Taketomi A, et al: Donor risk in adult-to-adult living donor liver transgplantation: impact of left lobe graft. Cherqui D, et al: Laparoscopic living donor hepatectomy for liver transplantation in children. Samstein B, et al: Fully laparoscopic left-sided donor hepatectomy is safe and associated with shorter hospital stay and earlier return to work: a comparative study. Tzakis A, et al: Orthotopic liver transplantation with preservation of the inferior vena cava. Belghiti J, et al: A new technique of side to side caval anastomosis during orthotopic hepatic transplantation without inferior vena caval occlusion. Cherqui D, et al: Liver transplantation with preservation of portacaval flow: comparison with the conventional technique. Arcari M, et al: An investigation into the risk of air embolus during veno-venous bypass in orthotopic liver transplantation. Veroli P, et al: Does adult liver transplantation without venovenous bypass result in renal failure Grande L, et al: Effect of venovenous bypass on perioperative renal function in liver transplantation: results of a randomized, controlled trial. Paskonis M, et al: Surgical strategies for liver transplantation in the case of portal vein thrombosis-current role of cavoportal hemitransposition and renoportal anastomosis. Quintini C, et al: Safety and effectiveness of renoportal bypass in patients with complete portal vein thrombosis: an analysis of 10 patients. Aggarwal S, et al: Postreperfusion syndrome: hypotension after reperfusion of the transplanted liver. Hilmi I, et al: the impact of postreperfusion syndrome on shortterm patient and liver allograft outcome in patients undergoing orthotopic liver transplantation. Uemura T, et al: Liver retransplantation for primary nonfunction: analysis of a 20-year single-center experience. Totsuka E, et al: Influence of high donor serum sodium levels on early postoperative graft function in human liver transplantation: effect of correction of donor hypernatremia. Yersiz H, et al: Correlation between donor age and the pattern of liver graft recovery after transplantation. Gunsar F, et al: Late hepatic artery thrombosis after orthotopic liver transplantation. Concejero A, et al: Donor graft outflow venoplasty in living donor liver transplantation. Ko G-Y, et al: Endovascular treatment of hepatic venous outflow obstruction after living-donor liver transplantation. Wojcicki M, et al: Biliary tract complications after liver transplantation: a review. Zoepf T, et al: Diagnosis of biliary strictures after liver transplantation: which is the best tool Fan S-T, et al: Biliary reconstruction and complications of right lobe live donor liver transplantation. Soejima Y, et al: Biliary strictures in living donor liver transplantation: incidence, management, and technical evolution. Following discharge from the hospital, blood tests are performed once or twice weekly initially, with the interval between blood tests extending as the patient recovers. However, as shown in Table 52-2, the cause of graft dysfunction also changes as the time from transplantation increases. This is manifested by aminotransferase levels often as high as 1000 U/L in the first postoperative week. Typically, the aminotransferase levels start to recover in 1 to 2 days, along with stabilization of the international normalized ratio and gradual improvement in serum bilirubin level. For this reason it is common practice to decline donor organs with greater than 25% macrovesicular fat content on pretransplant assessment. Biliary strictures may also present in the early period with liver enzyme level abnormalities, typically in a cholestatic pattern. For the candidates with greatest urgency, mortality was 20% in the first 3 months. Table 52-1 lists the donor and recipient factors that influence patient and graft survival. One must be vigilant for the onset of urinary tract infections, wound infections, pneumonias, infected intravenous cannulae, and septicemia. Activation of T lymphocytes plays a central role in the immune response to an allogeneic transplanted tissue. Costimulatory signals differ both in their ability to increase or decrease T-cell activation and in their patterns of expression. T-lymphocyte activation occurs through a cascade of stimulatory or augmentative signals. These include, but are not limited to , varicella, zoster, measles, rotavirus, yellow fever, and oral polio vaccines. Note the lack of a ductular reaction, portal expansion,oredema(hematoxylinandeosinstains). Maintenance immunosuppressive therapy may be maintained at prior doses or increased while pulse corticosteroids are administered. Note the strong C4d immunolabeling of the endothelium of the portal microvasculature and sinusoids. ChronicDuctopenicRejection Chronic ductopenic rejection denotes damage and eventual loss of bile ducts in portal tracts. Chronic ductopenic rejection occurs as a consequence of corticosteroid-resistant rejection or de novo. Given their potency and nonspecific mechanism of action, they are also unfortunately associated with significant side effects, thus limiting their use. A typical regimen comprises a calcineurin inhibitor (most commonly tacrolimus), a nucleotide synthesis inhibitor (most commonly mycophenolate mofetil), and a corticosteroid. During maintenance therapy in the first year, total immunosuppression is progressively reduced while liver biochemistry is monitored. Some programs maintain long-term low-dose prednisone therapy in recipients who underwent transplant for autoimmune indications. Many programs continue use of a second agent, commonly either mycophenolate mofetil or mycophenolic acid, which permits use of a lower dose of tacrolimus. Corticosteroids Corticosteroids interact with the immune system at multiple levels to exert their antiinflammatory and immunomodulatory effects. They are thus used for induction and maintenance of immunosuppression, and treatment of allograft rejection. The nucleotide synthesis inhibitors execute their immunosuppressive effects by interfering with the proliferative phase in the cell cycle, reducing the expansion of the population of activated T and B cells. Although vestigial esophageal or gastric varices may remain, variceal hemorrhage is very rare, unless it is in the presence of a new source of portal hypertension such as portal vein thrombosis. Persistent ascites is usually accompanied by portal hypertension when studied by transjugular pressure measurements. BiliaryComplications the bile ducts in the allograft are very sensitive to ischemia. Ischemic insults, particularly at the time of cold ischemia, can result in biliary leaks, biliary tract strictures, and bile duct stones. Consequently, biliary complications are more common in patients who receive an allograft from a cardiac death donor. Most strictures of the bile duct to bile duct anastomosis can be managed successfully with endoscopic retrograde cholangiopancreatography.
Trimethoprimsulfamethoxazole is widely used in developing countries as chronic prophylaxis against opportunistic infections arteries replacement order procardia with visa, with some success cardiovascular disease treatment methods discount 30 mg procardia fast delivery,485-487 and hepatotoxic reactions with the use of the drug in these populations have been reported cardiovascular disease gender differences order cheapest procardia. The fluoroquinolones currently available for use in United States include ciprofloxacin cardiovascular operating room nurse purchase procardia 30 mg overnight delivery, gemifloxacin arteries and veins of the heart buy discount procardia on-line, levofloxacin cardiovascular system in spanish generic procardia 30mg with mastercard, moxifloxacin, norfloxacin, and ofloxacin. The mechanism of the steatosis and toxicity appeared to be inhibition of mitochondrial fatty acid oxidation488 and was probably dose related. Intravenously administered tetracycline is rarely used today, and the incidence of hepatotoxicity from orally administered low doses of tetracyclines is extremely low. Other Antibiotics Nitrofurantoin, still used as a long-term urinary tract infection antimicrobial, was reported in 1980 to cause acute and chronic liver disease. Quinupristin-dalfopristin is a relatively new streptogramin antibiotic for vancomycin-resistant enterococci and resistant staphylococcal infections501 that caused hyperbilirubinemia when given to liver transplant recipients. Hepatic dysfunction is listed as an adverse reaction in the Epocrates database but no literature citations could be found. Presentation was at between 2 weeks and 13 weeks and was not correlated with the degree of platelet inhibition. Hepatotoxicity attributable to warfarin is rare522; case reports are often following phenprocoumon exposure. Many of the angiotensin-converting enzyme inhibitors have been shown to have a low incidence of causing cholestatic hepatitis,528 including captopril,529 enalipril,530 lisinopril,531 fosinopril,532 and ramipril. Deaths have been reported with use of enalapril534 and lisinopril531; in the latter case, death was attributed to a perforated ulcer while the cholestasis was abating. Patients who develop hepatitis caused by an angiotensin-converting enzyme inhibitor may develop crossreactivity when switched to an alternative angiotensin-converting enzyme inhibitor. The onset of clinical illness was always just a few weeks after the start of therapy and resolution was relatively rapid after discontinuation of use of the drug. The incidence of this reaction appears to be low, and deaths have not been reported. Antiarrhythmic Drugs Amiodarone is a highly effective and widely used iodinated benzofuran antiarrhythmic that has long been known to cause liver injury. An acute hepatitis can occur within 24 hours of the start of parenteral therapy543 but the incidence of this is difficult to assess because the drug is usually used during cardiac arrests and most patients do not survive. Although adaptation may occur, with normalization of values on continued use, use of the drug is often stopped because of toxic effects on other organs and death from heart disease. The drug and its metabolite remain in the liver and plasma for long periods and can cause persistent abnormalities for many months after cessation of therapy. The drug and metabolite accumulate in the liver because they are amphiphilic, becoming trapped in lysosomes and subsequently inhibiting phospholipases. Although only mild liver test abnormalities are listed in the Epocrates database for procainamide, the drug has been reported to cause intrahepatic cholestasis in a number of cases,281 often with granulomas. The drug is much more likely to cause a systemic lupus-like reaction than to cause hepatotoxicity. Considering the wide use of these agents, it appears that hepatotoxicity is very rare. Ca2+ Channel Blockers these agents appear to have a very low incidence of hepatotoxicity, with only verapamil and diltiazem listed in the Epocrates database. Still, nifedipine has been reported to cause acute hepatitis with immune features,559 with the last report published in 1992. Considering the widespread use of these agents in relatively sick patients, including those with liver disease, it is clear that they have very little hepatotoxicity. The uricosuric diuretic tienilic acid was withdrawn from the market in 1979 because of a large number of cases of acute and chronic hepatitis, most likely the result of an immune-mediated process. Hydrazine-induced hepatotoxicity spans the spectrum of liver disease, including acute hepatitis, cholestatic hepatitis, granulomatous hepatitis, and hepatitis with hypersensitivity features. Most case reports of hepatotoxicity from dihydralazine568 show classic centrilobular necrosis. From a historical perspective, -methyldopa (Aldomet) was one of the first drugs in widespread use that was noted to be hepatotoxic, but with a low enough incidence that it was not withdrawn from the market. It remains a popular choice in hypertension in pregnancy given its record of safety in pregnancy and breast-feeding. All forms of liver injury, including acute hepatitis, chronic hepatitis, cholestatic hepatitis, fulminant liver failure, and cirrhosis, have been associated with its use. Because of the presence of autoimmune features, treatment with oral steroids has been tried, with full recovery. Bosentan is an orally available benzenesulfonamide designed to potently inhibit both endothelin receptor A and endothelin receptor B. Cholesterol-Lowering Agents the introduction of the statins has had a major impact on the therapy for hypercholesterolemia and heart disease, making these agents among the most widely prescribed medications. However, because these are long-term medications, there was early concern about ocular, muscle, and liver toxicities that had been seen with previous inhibitors of cholesterol synthesis. There were also a number of severe cases of acute hepatitis and cholestatic injury. Unfortunately, following these recommendations would deny many patients with high cholesterol levels the benefit of these drugs because these patients often have increased levels of serum aminotransferases as part of their metabolic syndrome. Studies in specific groups, including children with familial hypercholesterolemia,582 obese patients,583 elderly patients,584 and patients with increases before therapy,585 showed that all tolerated statin therapy with a low incidence of side effects. It is still recommended that liver function test results and creatine kinase levels be monitored at the baseline, at 3 months, and then every 6 months,586 although it has not been demonstrated that this will identify those patients at risk of, nor reduce the occurrence of, severe liver or muscle toxicity. There are also warnings concerning the combination of statins with gemfibrozil, niacin, amiodarone, and verapamil. Statins were incriminated in 11 cases, with a mean serum total bilirubin level of 6. Given the vast number of prescriptions written for this class of drug, more than 142 million in the United States in 2008 alone, the relatively small number of published case reports is a testament to the hepatic safety of statins. Despite differences in pharmacokinetics, lipophilicity, and degree of hepatic metabolism,590 all statins appear capable of causing rare but significant hepatotoxicity. Presenting symptoms have generally been consistent with an acute hepatitis, including jaundice, anorexia, nausea, abdominal pain, fatigue, and pruritus. The time from cessation of statin use until resolution of hepatotoxicity ranges from several weeks to 6 months. In cases of mixed injury, the peak serum total bilirubin level has been reported as high as 25 mg/dL but in most cases the total bilirubin levels are 5 mg/dL to 10 mg/dL. The portal inflammation typically includes lymphocytes, and although eosinophils were noted in a few cases, they are not commonly prominent. Changes on liver biopsy may not be due to statins, however, because these patients may have preexisting underlying fatty liver disease and/or liver fibrosis. Statin-induced liver injury may occasionally present with an autoimmune phenotype. These cases could represent sporadic autoimmune hepatitis in someone who happened to be prescribed a statin, although the evidence for statins serving as a trigger is strong. As a drug class, statins are remarkably safe, including in patients with chronic liver disease or a history of elevated liver function test values. Most of the participants in the study had chronic liver disease from nonalcoholic fatty liver disease (64. One patient with cirrhosis treated with ezetimibe and simvastatin died and one patient with rheumatoid arthritis treated with leflunomide and lovastatin underwent a liver transplant. The following are recommendations from the National Lipid Association Safety Task Force regarding the safety of statins with a focus on patients with chronic liver disease596: (1) chronic liver disease is not a contraindication to statin therapy; (2) compensated cirrhosis is not a contraindication to statin therapy; (3) statins can be prescribed safely to patients with nonalcoholic fatty liver disease. Furthermore, patients should not reinitiate statin therapy if they experienced prior liver test value elevations presumably attributable to statin use. Fenofibrate has been used for decades and is effective for the management of hypertriglyceridemia. It has been reported to rarely cause an autoimmune hepatitis with ductopenia and fibrosis. There is some indication that toxicity may be dose related,281 but the mechanism of liver injury has never been clarified. Although the incidence of hepatotoxicity varies for different agents, the overall incidence of overt dysfunction is low (less than 0. Benoxaprofen proved to be an agent that caused liver injury with a high incidence and high mortality, prompting its withdrawal from medical use. These include the connective tissue disorders rheumatoid arthritis, systemic lupus erythematosus, and juvenile rheumatoid arthritis. However, the increased incidence in this subgroup is probably explained largely by the higher doses used in treating these conditions, rather than an intrinsic susceptibility, although the cytokine milieu in systemic inflammatory diseases may predispose to hepatotoxicity. In patients who develop Reye syndrome, aspirin intake appears to be one of the-probably the most common-triggers for the development of its characteristic features: namely, a microvesicular hepatic steatosis and acute encephalopathy. This occurs in the setting of a febrile illness in children, most commonly induced by a viral infection. The underlying predisposing condition is as yet unclear but may involve congenital mitochondrial enzyme defects or deficiencies, the effect of which is exacerbated by the use of aspirin. From the ultrastructural histologic features, the site of injury appears to be the mitochondria. Other mechanisms that have been postulated include lipid peroxidation, hydroxyl radical scavenging, and injury to the hepatocyte membrane. Aspirin hepatotoxicity is rapidly reversible when use of the drug is discontinued. Aspirin overdose is managed by discontinuation of use of the drug, with supportive care in the rare individual who has severe hepatotoxicity. If aspirin is absolutely essential in the treatment of the individual, an attempt may be made to restart use of the drug at a lower dose after the liver function test values have returned to normal. Close monitoring of the liver function test values in this rechallenge is necessary. Diflunisal (Dolobid) is a difluorophenyl derivative of salicylic acid that has been reported to cause a cholestatic and mixed hepatocellular type of injury. There are relatively few reports of indomethacin-related hepatic injury compared with injuries of other organs caused by this drug. Features are usually nonspecific, with laboratory values suggesting hepatocellular injury, and much less often concomitant cholestasis. Sulindac (Clinoril) is also an indole derivative of acetic acid and therefore has some structural similarities to indomethacin. Eosinophilia tends to be more common when the pattern of injury is cholestatic than when it is primarily hepatocellular. However, metabolic idiosyncrasy seemed to be the more logical explanation in other cases. Liver test abnormalities favor hepatocellular or mixed hepatitis in most cases, and cases mimicking autoimmune hepatitis with antinuclear antibody positivity have been described. Other features may include granulomas, cholestasis, hepatic eosinophilia, and chronic hepatitis. Rarely, the use of diclofenac has been thought to trigger development of autoimmune hepatitis. Animal studies demonstrate acetaminophen-induced liver injury is mediated through reactive oxygen species and hepatocyte apoptosis. Reactive oxygen species are associated with mitochondrial damage and the activation of caspases. Further support of the role of the oxidative stress response as an important mechanism in acetaminophen hepatotoxicity is demonstrated in a study of metallothioneinknockout mice. More lipid peroxidation was present in metallothionein-knockout mice as evidenced by immunohistochemical localization of 4-hydroxynonenal and malondialdehyde protein adducts. Other transcription factors that protect against oxidative injury have been reported to be associated with acetaminophen toxicity in mice. Other enzymes and pathways associated with acetaminophen-induced liver injury include activation of the glycogen synthase kinase 3 and c-Jun N-terminal kinase pathways. The innate immune system and natural killer cell activation and increase in interferon- level have been shown to play a role in progression and severity of acetaminophen hepatotoxicity. Although acetaminophen plasma levels are helpful to guide treatment with N-acetylcysteine, overdose may be undetected when plasma levels are low, especially in individuals with long-term or unintentional overdose. Causality assessment of hepatotoxicity in the setting of cancer chemotherapy is often difficult for the following reasons: 1. Abnormal liver test results may result from metastasis or infiltration of the liver parenchyma or biliary tree by tumor. Immunosuppression may result in sepsis and shock, with its attendant cytokine-induced effects on the liver, such as cholestasis. Occasionally the liver itself may be opportunistically infected, or transfusion may result in viral hepatitis. Examples include the direct effects of radiation and graft-versus-host disease in patients undergoing bone marrow or stem cell transplants. Drugs that have minimal hepatotoxic potential when used alone may produce severe liver disease when used in combination with other chemotherapeutic agents or with radiation therapy. Liver biopsy, which might help in differential diagnosis, is often contraindicated because of thrombocytopenia and coagulation abnormalities caused by treatment.


















