Cialis Super Active

Richard A. Humes, MD
- Professor
- Department of Pediatrics
- Wayne State University
- Chief
- Division of Cardiology
- Children? Hospital of Michigan
- Detroit, Michigan
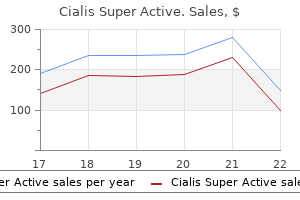
Ketamine may increase systemic arterial pressure and has been associated with hallucinatory responses erectile dysfunction treatment raleigh nc order cialis super active 20 mg with visa. The shorter-acting agents etomidate and propofol have been used for both induction and maintenance of anesthesia in ventilated patients because they have fewer adverse hemodynamic effects erectile dysfunction treatment canada buy generic cialis super active online, but both are significantly more expensive than older agents erectile dysfunction effects on women order cialis super active 20 mg mastercard. Great care must be taken to avoid the use of neuromuscular paralysis during intubation of patients with renal failure erectile dysfunction circumcision generic 20mg cialis super active fast delivery, tumor lysis syndrome erectile dysfunction in 40s discount 20 mg cialis super active with visa, crush injuries erectile dysfunction symptoms causes and treatments buy 20 mg cialis super active overnight delivery, medical conditions associated with elevated serum potassium levels, and muscular dystrophy syndromes; in particular, the use of agents whose mechanism of action includes depolarization at the neuromuscular junction, such as succinylcholine chloride, must be avoided. This condition is well tolerated when care is taken to avoid excess acidosis by pH buffering. The trigger, either an inspiratory effort or a timebased signal, defines what the ventilator senses to initiate an assisted breath. For example, in volume-cycled ventilation, inspiration ends when a specific tidal volume is delivered. Alveoli tend to close if the distending pressure falls below the lower inflection point (A), whereas they overstretch if the pressure within them is higher than that of the upper inflection point (B). Collapse and opening of ventilated alveoli are associated with poor outcomes in patients with acute respiratory failure. Protective ventilation (purple shaded area), using a lower tidal volume (6 mL/kg of ideal body weight) and maintaining positive end-expiratory pressure to prevent overstretching and collapse/opening of alveoli, has resulted in improved survival rates among patients receiving mechanical ventilatory support. Every breath delivered, whether patient- or timer-triggered, consists of the operator-specified tidal volume. Ventilatory rate is determined either by the patient or by the operator-specified backup rate, whichever is of higher frequency. If the patient fails to initiate a breath, the ventilator delivers a fixed-tidal-volume breath and resets the internal timer for the next inspiratory cycle. Consequently, the airway pressure may exceed the inspiratory pressure limit, the ventilator-assisted breath will be aborted, and minute volume may drop below that programmed by the operator. It provides graded assistance and differs from the other two modes in that the operator sets the pressure level (rather than the volume) to augment every spontaneous respiratory effort. Although their use in acute respiratory failure is limited, the following modes have been used with varying levels of enthusiasm and adoption. Pressure-control ventilation (Pcv) this form of ventilation is timetriggered, time-cycled, and pressure-limited. Since the inspiratory pressure is specified by the operator, tidal volume and inspiratory flow rate are dependent, rather than independent, variables and are not operator-specified. This approach increases mean distending pressures without increasing peak airway pressures. The ventilator provides fresh gas to the breathing circuit with each inspiration and sets the circuit to a constant, operatorspecified pressure. Nonconventional Ventilatory Strategies Several nonconventional strategies have been evaluated for their ability to improve oxygenation and reduce mortality rates in patients with advanced hypoxemic respiratory failure. Although case reports and small uncontrolled cohort studies have shown benefit, randomized controlled trials have failed to demonstrate consistent improvements in outcome with most of these strategies. Currently, these approaches should be thought of as "salvage" techniques and considered for patients with hypoxemia refractory to conventional therapy. Prone positioning of patients with refractory hypoxemia has also been explored because, in theory, lying prone should improve ventilationperfusion matching. Several randomized trials in patients with acute lung injury did not demonstrate a survival advantage with prone positioning despite demonstration of a transient physiologic benefit. The administration of nitric oxide gas, which has bronchodilator and pulmonary vasodilator effects when delivered through the airways and improves arterial oxygenation in many patients with advanced hypoxemic respiratory failure, also failed to improve outcomes in these patients with acute lung injury. With the application of these techniques, the mortality rate among patients with acute hypoxemic respiratory failure has decreased to ~30% from close to 50% a decade ago. As improvement in respiratory function is noted, the first priority is to reduce the level of mechanical ventilatory support. Patients on full ventilatory support should be monitored frequently, with the goal of switching to a mode that allows for weaning as soon as possible. Immobilized patients receiving mechanical ventilatory support are at risk for deep venous thrombosis and decubitus ulcers. Venous thrombosis should be prevented with the use of subcutaneous heparin and/or pneumatic compression boots. Fractionated low-molecularweight heparin appears to be equally effective for this purpose. To help prevent decubitus ulcers, frequent changes in body position and the use of soft mattress overlays and air mattresses are employed. Histamine-receptor (H2-receptor) antagonists, antacids, and cytoprotective agents such as sucralfate have all been used for this purpose and appear to be effective. Nutritional support by enteral feeding through either a nasogastric or an orogastric tube should be initiated and maintained whenever possible. Delayed gastric emptying is common in critically ill patients taking sedative medications but often responds to promotility agents such as metoclopramide. Pulmonary complications include barotrauma, nosocomial pneumonia, oxygen toxicity, tracheal stenosis, and deconditioning of respiratory muscles. Barotrauma and volutrauma overdistend and disrupt lung tissue; may be clinically manifest by interstitial emphysema, pneumomediastinum, subcutaneous emphysema, or pneumothorax; and can result in the liberation of cytokines from overdistended tissues, further promoting tissue injury. Intubated patients are at high risk for ventilator-associated pneumonia as a result of aspiration from the upper airways through small leaks around the endotracheal tube cuff; the most common organisms responsible for this condition are Pseudomonas aeruginosa, enteric gram-negative rods, and Staphylococcus aureus. Given the high associated mortality rates, early initiation of empirical antibiotics directed against likely pathogens is recommended. Hypotension resulting from elevated intrathoracic pressures with decreased venous return is almost always responsive to intravascular volume repletion. In patients who are judged to have respiratory failure on the basis of alveolar edema but in whom the cardiac or pulmonary origin of the edema is unclear, hemodynamic monitoring with a pulmonary arterial catheter may be of value in helping to clarify the cause of the edema. Gastrointestinal effects of positive-pressure ventilation include stress ulceration and mild to moderate cholestasis. Although the predictive capacities of multiple clinical and physiologic variables have been explored, the consensus from a ventilatory weaning task force cites the following conditions as indicating amenability to weaning: (1) Lung injury is stable or resolving. Often, this treatment consists of a combination of a benzodiazepine and an opiate administered intravenously. Medications commonly used for this purpose include lorazepam, midazolam, diazepam, morphine, and fentanyl. In these instances, critical care personnel must decide whether and when to perform a tracheostomy. A tracheostomy is thought to be more comfortable, to require less sedation, and to provide a more secure airway and may also reduce weaning time. In patients with long-term tracheostomy, complex complications include tracheal stenosis, granulation, and erosion of the innominate artery. Whether it is completed at the bedside or as an operative procedure depends on local resources and experience. Unfortunately, close to 2% of ventilated patients may ultimately become dependent on ventilatory support to maintain life. Most of these patients remain in chronic care institutions, although some with strong social, economic, and family support may live a relatively fulfilling life with at-home ventilation. In addition, other factors must be taken into account, such as the possible difficulty of replacing the tube if that maneuver is required. The fundamental approach to management, therefore, is to recognize overt and impending shock in a timely fashion and to intervene emergently to restore perfusion. Doing so often requires the expansion or reexpansion of intravascular blood volume. Multiple classification schemes have been developed in an attempt to synthesize the seemingly dissimilar processes leading to shock. Strict adherence to a classification scheme may be difficult from a clinical standpoint because of the frequent combination of two or more causes of shock in any individual patient, but the classification shown in Table 324-1 provides a useful reference point from which to discuss and further delineate the underlying processes. Maier Shock is the clinical syndrome that results from inadequate tissue perfusion. Irrespective of cause, the hypoperfusion-induced imbalance between the delivery of and requirements for oxygen and substrate leads to cellular dysfunction. The clinical manifestations of shock are also the result, in part, of autonomic neuroendocrine responses to hypoperfusion as well as the breakdown in organ function induced by severe cellular dysfunction. Systemic vascular resistance is determined primarily by the luminal diameter of arterioles. The metabolic rates of the heart and brain are high, and their stores of energy substrate are low. As shock progresses, these vasodilator metabolites override vasomotor tone, causing furConsumptive ther hypotension and hypoperfusion. Normal cellular transmembrane potential falls, and there is an associated increase in continuous supply of oxygen and nutrients, and neither tolerates severe intracellular sodium and water, leading to cell swelling that interferes ischemia for more than brief periods (minutes). In a preterminal event, homeothe maintenance of blood flow over a wide range of perfusion pres- stasis of calcium via membrane channels is lost with flooding of calcium sures) is critical in sustaining cerebral and coronary perfusion despite into the cytosol and concomitant extracellular hypocalcemia. Efferent sympathetic fibers release Hypovolemia, hypotension, and hypoxia are sensed by baroreceptors norepinephrine, which acts primarily on 1 receptors as one of the and chemoreceptors that contribute to an autonomic response that most fundamental compensatory responses to reduced perfusion pres- attempts to restore blood volume, maintain central perfusion, and sure. Other constrictor substances that are increased in most forms of mobilize metabolic substrates. Release of norepinephrine from adrenergic neurons induces adrenal medulla, and the concentrations of these catecholamines in significant peripheral and splanchnic vasoconstriction, a major conthe bloodstream rise. The effects of circulating epinephrine released by strictors and vasodilators influences the microcirculation and deter- the adrenal medulla in shock are largely metabolic, causing increased mines local perfusion. However, epinephrine also inhibits production and release of permeability; the diffusion of oxygen, carbon dioxide, nutrients, and inflammatory mediators through stimulation of -adrenergic recepproducts of metabolism through the interstitium; and the exchange tors on innate immune cells. This stimulates cortisol secretion late stages of all forms of shock results in the derangement of cellular that contributes to decreased peripheral uptake of glucose and amino metabolism that is ultimately responsible for organ failure. Increased the endogenous response to mild or moderate hypovolemia is an pancreatic secretion of glucagon during stress accelerates hepatic gluattempt at restitution of intravascular volume through alterations in coneogenesis and further elevates blood glucose concentration. Constriction of arterioles leads hormonal actions act synergistically to increase blood glucose for both to reductions in both the capillary hydrostatic pressure and the num- selective tissue metabolism and the maintenance of blood volume. The importance of the cortisol response to stress is illustrated by the profound circulatory collapse that occurs in patients with adrenocortical insufficiency (Chap. Metabolic changes (including hyperglycemia and elevations in the products of glycolysis, lipolysis, and proteolysis) raise extracellular osmolarity, leading to an osmotic gradient that increases interstitial and intravascular volume at the expense of intracellular volume. Vasopressin has a direct action on vascular smooth muscle, contributing to vasoconstriction, and acts on the distal renal tubules to enhance water reabsorption. Cardiac output, the major determinant of tissue perfusion, is the product of stroke volume and heart rate. Hypovolemia leads to decreased ventricular preload that, in turn, reduces the stroke volume. An increase in heart rate is a useful but limited compensatory mechanism to maintain cardiac output. A shock-induced reduction in myocardial compliance is frequent, reducing ventricular end-diastolic volume and, hence, stroke volume at any given ventricular filling pressure. Restoration of intravascular volume may return stroke volume to normal but only at elevated filling pressures. The resistance to ventricular ejection is significantly influenced by the systemic vascular resistance, which is elevated in most forms of shock. However, resistance is decreased in the early hyperdynamic stage of septic shock or neurogenic shock (Chap. The venous system contains nearly two-thirds of the total circulating blood volume, most in the small veins, and serves as a dynamic reservoir for autoinfusion of blood. Active venoconstriction as a consequence of -adrenergic activity is an important compensatory mechanism for the maintenance of venous return and, therefore, of ventricular filling during shock. By contrast, venous dilation, as occurs in neurogenic shock, reduces ventricular filling and hence stroke volume and potentially cardiac output. Shockinduced tachypnea reduces tidal volume and increases both dead space and minute ventilation. Recumbency and involuntary restriction of ventilation secondary to pain reduce functional residual capacity and may lead to atelectasis. These disorders are characterized by noncardiogenic pulmonary edema secondary to diffuse pulmonary capillary endothelial and alveolar epithelial injury, hypoxemia, and bilateral diffuse pulmonary infiltrates. Loss of surfactant and lung volume in combination with increased interstitial and alveolar edema reduces lung compliance. The work of breathing and the oxygen requirements of respiratory muscles increase. Acute tubular necrosis is now more frequently seen as a result of the interactions of shock, sepsis, the administration of nephrotoxic agents (such as aminoglycosides and angiographic contrast media), and rhabdomyolysis; the latter may be particularly severe in skeletal muscle trauma. The physiologic response of the kidney to hypoperfusion is to conserve salt and water. Toxic injury causes necrosis of tubular epithelium and tubular obstruction by cellular debris with back leak of filtrate. Through the citric acid cycle, alanine in conjunction with lactate, which is converted from pyruvate in the periphery in the presence of oxygen deprivation, enhances the hepatic production of glucose. With reduced availability of oxygen, the breakdown of glucose to pyruvate, and ultimately lactate, represents an inefficient cycling of substrate with minimal net energy production. An elevated plasma lactate/pyruvate ratio is preferable to lactate alone as a measure of anaerobic metabolism and reflects inadequate tissue perfusion. Decreased clearance of exogenous triglycerides coupled with increased hepatic lipogenesis causes a significant rise in serum triglyceride concentrations.
The nonlinearity and multiplicity of these interactions have made it difficult to interpret the roles played by individual mediators in both tissues and blood erectile dysfunction treatment options exercise safe 20 mg cialis super active. The result is activation of both extrinsic and intrinsic clotting pathways drugs used for erectile dysfunction cialis super active 20 mg low cost, culminating in the generation of fibrin list all erectile dysfunction drugs discount cialis super active 20mg without prescription. Thus vacuum pump for erectile dysfunction in pakistan buy 20mg cialis super active visa, there may be a striking propensity toward intravascular fibrin deposition erectile dysfunction treatment diabetes purchase cialis super active 20 mg amex, thrombosis erectile dysfunction age 35 order generic cialis super active line, and bleeding; this propensity has been most apparent in patients with intravascular endothelial infections such as meningococcemia (Chap. Local control mechanisms Host recognition of invading microbes within subepithelial tissues typically ignites immune responses that rapidly kill the invaders and then subside to allow tissue recovery. The forces that put out the fire and clean up the battleground include molecules that neutralize or inactivate microbial signals. Systemic control mechanisms the signaling apparatus that links microbial recognition to cellular responses in tissues is less active in the blood. Glucocorticoids inhibit cytokine synthesis by monocytes in vitro; the increase in blood cortisol levels that occurs early in the systemic response presumably plays a similarly inhibitory role. Other acute-phase proteins are protease inhibitors or antioxidants; these may neutralize potentially harmful molecules released from neutrophils and other inflammatory cells. It may thus be said that both local and systemic responses to infectious agents benefit the host in important ways. Most of these responses and the molecules responsible for them have been highly conserved during animal evolution and therefore may be adaptive. Although high concentrations of both pro- and anti-inflammatory molecules are found, the net mediator balance in the plasma of these extremely sick patients seems to be anti-inflammatory. In addition, regulated cell-adhesion molecules promote the adherence of neutrophils to endothelial cells. Tissue oxygenation may decrease as the number of functional capillaries is reduced by luminal obstruction due to swollen endothelial cells, decreased deformability of circulating erythrocytes, leukocyteplatelet-fibrin thrombi, or compression by edema fluid. On the other hand, studies using orthogonal polarization spectral imaging of the microcirculation in the tongue found that sepsis-associated derangements in capillary flow could be reversed by applying acetylcholine to the surface of the tongue or by giving nitroprusside intravenously; these observations suggest a neuroendocrine basis for the loss of capillary filling. The local accumulation of lactic acid, a consequence of increased glycolysis, may decrease extracellular pH and contribute to the slowdown in cellular metabolism that occurs within affected tissues. These points suggest that organ dysfunction during severe sepsis has a basis that is principally biochemical, not structural. Before this vasodilatory phase, many patients experience a period during which oxygen delivery to tissues is compromised by myocardial depression, hypovolemia, and other factors. During this "hypodynamic" period, the blood lactate concentration is elevated and central venous oxygen saturation is low. Fluid administration is usually followed by the hyperdynamic vasodilatory phase, during which cardiac output is normal (or even high) and oxygen consumption declines despite adequate oxygen delivery. The blood lactate level may be normal or increased, and normalization of central venous oxygen saturation may reflect improved oxygen delivery, decreased oxygen uptake by tissues, or left-to-right shunting. Prominent hypotensive molecules include nitric oxide, -endorphin, bradykinin, platelet-activating factor, and prostacyclin. In most patients infected with other gram-negative bacteria, in contrast, circulating bacteria or bacterial molecules may reflect uncontrolled infection at a local tissue site and have little or no direct impact on distant organs; in these patients, inflammatory mediators or neural signals arising from the local site seem to be the key triggers for severe sepsis and septic shock. In a large series of patients with positive blood cultures, the risk of developing severe sepsis was strongly related to the site of primary infection: bacteremia arising from a pulmonary or abdominal source was eightfold more likely to be associated with severe sepsis than was bacteremic urinary tract infection, even after the investigators controlled for age, the kind of bacteria isolated from the blood, and other factors. A third pathogenesis may be represented by severe sepsis due to superantigen-producing S. Genetic factors are probably important as well, yet despite much study very few allelic polymorphisms have been associated with sepsis severity in more than one or two analyses. The rate at which severe sepsis develops may differ from patient to patient, and there are striking individual variations in presentation. For example, some patients with sepsis are normo- or hypothermic; the absence of fever is most common in neonates, in elderly patients, and in persons with uremia or alcoholism. Hyperventilation, producing respiratory alkalosis, is often an early sign of the septic response. Disorientation, confusion, and other manifestations of encephalopathy may also develop early on, particularly in the elderly and in individuals with preexisting neurologic impairment. A cutaneous lesion seen almost exclusively in neutropenic patients is ecthyma gangrenosum, often caused by P. This bullous lesion surrounded by edema undergoes central hemorrhage and necrosis. Hemorrhagic or bullous lesions in a septic patient who has recently eaten raw oysters suggest V. Generalized erythroderma in a septic patient suggests the toxic shock syndrome due to S. Gastrointestinal manifestations such as nausea, vomiting, diarrhea, and ileus may suggest acute gastroenteritis. Hepatocellular or canalicular dysfunction appears to underlie most cases, and the results of hepatic function tests return to normal with resolution of the infection. Serum albumin levels decline as a result of decreased hepatic synthesis and the movement of albumin into interstitial spaces. Increasing alveolar epithelial injury and capillary permeability result in increased pulmonary water content, which decreases pulmonary compliance and interferes with oxygen exchange. Sepsis-induced hypotension (see "Septic Shock," above) usually results initially from a generalized maldistribution of blood flow and blood volume and from hypovolemia that is due, at least in part, to diffuse capillary leakage of intravascular fluid. Other factors that may decrease effective intravascular volume include dehydration from antecedent disease or insensible fluid losses, vomiting or diarrhea, and polyuria. Indeed, normal or increased cardiac output and decreased systemic vascular resistance distinguish septic shock from cardiogenic, extracardiac obstructive, and hypovolemic shock; other processes that can produce this combination include anaphylaxis, beriberi, cirrhosis, and overdoses of nitroprusside or narcotics. Depression of myocardial function, manifested as increased enddiastolic and systolic ventricular volumes with a decreased ejection fraction, develops within 24 h in most patients with severe sepsis. Cardiac output is maintained despite the low ejection fraction because ventricular dilation permits a normal stroke volume. Although myocardial dysfunction may contribute to hypotension, refractory hypotension is usually due to low systemic vascular resistance, and 1755 death most often results from refractory shock or the failure of multiple organs rather than from cardiac dysfunction per se. Adrenal Insufficiency the diagnosis of adrenal insufficiency may be very difficult in critically ill patients. Whereas a plasma cortisol level of 15 g/mL (10 g/mL if the serum albumin concentration is <2. Some classic features of adrenal insufficiency, such as hyponatremia and hyperkalemia, are usually absent; others, such as eosinophilia and modest hypoglycemia, may sometimes be found. Renal Complications Oliguria, azotemia, proteinuria, and nonspecific urinary casts are frequently found. Most renal failure is due to acute tubular necrosis induced by hypovolemia, arterial hypotension, or toxic drugs, although some patients also have glomerulonephritis, renal cortical necrosis, or interstitial nephritis. Drug-induced renal damage may greatly complicate therapy, particularly when hypotensive patients are given aminoglycoside antibiotics. Nosocomial sepsis following acute renal injury is associated with a high mortality rate. Neurologic Complications Delirium (acute encephalopathy) is often an early manifestation of sepsis. When the septic illness lasts for weeks or months, "critical illness" polyneuropathy may prevent weaning from ventilatory support and produce distal motor weakness. Recent studies have documented long-term cognitive loss in survivors of severe sepsis. Immunosuppression Patients with severe sepsis often become profoundly immunosuppressed. Manifestations include loss of delayedtype hypersensitivity reactions to common antigens, failure to control the primary infection, and increased risk for secondary infections. Approximately onethird of patients experience reactivation of herpes simplex virus, varicellazoster virus, or cytomegalovirus infections; the latter are thought to contribute to adverse outcomes in some instances. Evaluation of arterial blood gases reveals hypoxemia that is initially correctable with supplemental oxygen but whose later refractoriness to 100% oxygen inhalation indicates right-to-left shunting. Severe infection may precipitate diabetic ketoacidosis that may exacerbate hypotension (Chap. Diagnostically sensitive findings in a patient with suspected or proven infection include fever or hypothermia, tachypnea, tachycardia, and leukocytosis or leukopenia (Table 325-1); acutely altered mental status, thrombocytopenia, an elevated blood lactate level, respiratory alkalosis, or hypotension also should suggest the diagnosis. Moreover, the systemic responses of uninfected patients with other conditions may be similar to those characteristic of sepsis. Examples include pancreatitis, burns, trauma, adrenal insufficiency, pulmonary embolism, dissecting or ruptured aortic aneurysm, myocardial infarction, occult hemorrhage, cardiac tamponade, postcardiopulmonary bypass syndrome, anaphylaxis, tumor-associated lactic acidosis, and drug overdose. Definitive etiologic diagnosis requires identification of the causative microorganism from blood or a local site of infection. At least two blood samples should be obtained (from two different venipuncture sites) for culture; in a patient with an indwelling catheter, one sample should be collected from each lumen of the catheter and another via venipuncture. In many cases, blood cultures are negative; this result can reflect prior antibiotic administration, the presence of slow-growing or fastidious organisms, or the absence of microbial invasion of the bloodstream. A large retrospective review of patients who developed septic shock found that the interval between the onset of hypotension and the administration of appropriate antimicrobial chemotherapy was the major determinant of outcome; a delay of as little as 1 h was associated with lower survival rates. Use of "inappropriate" antibiotics, defined on the basis of local microbial susceptibilities and published guidelines for empirical therapy (see below), was associated with fivefold lower survival rates, even among patients with negative cultures. It is therefore very important to promptly initiate empirical antimicrobial therapy that is effective against both gram-positive and gram-negative bacteria (Table 325-3). When culture results become available, the regimen can often be simplified because a single antimicrobial agent is usually adequate for the treatment of a known pathogen. Meta-analyses have concluded that, with one exception, combination antimicrobial therapy is not superior to monotherapy for treating gram-negative bacteremia; the exception is that aminoglycoside monotherapy for P. The chosen antimicrobial regimen should be reconsidered daily in order to provide maximal efficacy with minimal resistance, toxicity, and cost. The absence of an identified microbial pathogen is not necessarily an indication for discontinuing antimicrobial therapy because "appropriate" antimicrobial regimens seem to be beneficial in both culture-negative and culture-positive cases. Sites of occult infection should be sought carefully, particularly in the lungs, abdomen, and urinary tract. The possibility of paranasal sinusitis (often caused by gram-negative bacteria) should be considered if the patient has undergone nasal intubation or has an indwelling nasogastric or feeding tube. In the neutropenic patient, cutaneous sites of tenderness and erythema, particularly in the perianal region, must be carefully sought. Successful management requires urgent measures to treat the infection, to provide hemodynamic and respiratory support, and to remove or drain infected tissues. Empirical antifungal therapy with an echinocandin (for caspofungin: a 70-mg loading dose, then 50 mg daily), voriconazole (6 mg/kg q12h for 2 doses, then 3 mg/ kg q12h), or a lipid formulation of amphotericin B should be added if the patient is hypotensive, has been receiving broad-spectrum antibacterial drugs, or remains febrile 5 days after initiation of empirical antibacterial therapy. If the local prevalence of cephalosporinresistant pneumococci is high, add vancomycin. If the patient is allergic to -lactam drugs, vancomycin (15 mg/kg q12h) plus either moxifloxacin (400 mg q24h) or levofloxacin (750 mg q24h) should be used. Circulatory adequacy is assessed by measurement 1757 of arterial blood pressure and monitoring of parameters such as mentation, urine output, and skin perfusion. Indirect indices of oxygen delivery and consumption, such as central venous oxygen saturation, may also be useful. In about one-third of patients, hypotension and organ hypoperfusion respond to fluid resuscitation; a reasonable goal is to maintain a mean arterial blood pressure of >65 mmHg (systolic pressure >90 mmHg). If these guidelines cannot be met by volume infusion, vasopressor therapy is indicated (Chap. Titrated doses of norepinephrine should be administered through a central catheter. If myocardial dysfunction produces elevated cardiac filling pressures and low cardiac output, inotropic therapy with dobutamine is recommended. In patients with septic shock, plasma vasopressin levels increase transiently but then decrease dramatically. Early studies found that vasopressin infusion can reverse septic shock in some patients, reducing or eliminating the need for catecholamine pressors. Although vasopressin may benefit patients who require less norepinephrine, its role in the treatment of septic shock seems to be a minor one overall. Meta-analyses of recent clinical trials have concluded that hydrocortisone therapy hastens recovery from sepsis-induced hypotension without increasing long-term survival. Ventilator therapy is indicated for progressive hypoxemia, hypercapnia, neurologic deterioration, or respiratory muscle failure. Stress-ulcer prophylaxis with a histamine H2-receptor antagonist may decrease the risk of gastrointestinal hemorrhage in ventilated patients. Erythrocyte transfusion is generally recommended when the blood hemoglobin level decreases to 7 g/dL, with a target level of 9 g/dL in adults.
Discount cialis super active online amex. Flat Earth Zetetic Cosmogony by T. Winship.
Mild symptoms impotence causes buy 20 mg cialis super active free shipping, usually abdominal pain erectile dysfunction without pills order cheap cialis super active line, and recurrent acute pancreatitis are unusual does erectile dysfunction cause premature ejaculation purchase 20 mg cialis super active otc. Elevated serum levels of IgG4 provide a marker for the disease erectile dysfunction natural treatment order discount cialis super active, particularly in Western populations impotence symptoms signs buy cialis super active 20 mg mastercard. Characteristic histologic findings include extensive lymphoplasmacytic infiltrates with dense fibrosis around pancreatic ducts erectile dysfunction icd 9 code wiki cheap cialis super active 20 mg visa, as well as a lymphoplas- 2099 macytic infiltration, resulting in an obliterative phlebitis. Patients may respond dramatically to glucocorticoid therapy within a 2- to 4-week period. Prednisone is usually administered at an initial dose of 40 mg/d for 4 weeks followed by a taper of the daily dosage by 5 mg/wk based on monitoring of clinical parameters. A poor response to glucocorticoids over a 2- to 4-week period should raise suspicion of pancreatic cancer or other forms of chronic pancreatitis. A small number of patients responded favorably to 6-mercaptapurine, rituximab, cyclosporine, and cyclophosphamide. Relapse is common in type 1 patients, especially those with biliary tract strictures. Patients with refractory symptoms and strictures generally require immunomodulator therapy as noted above. Clinical Features of Chronic Pancreatitis Patients with chronic pancreatitis seek medical attention predominantly because of two symptoms: abdominal pain or maldigestion and weight loss. Eating may exacerbate the pain, leading to a fear of eating with consequent weight loss. Maldigestion is manifested as chronic diarrhea, steatorrhea, weight loss, and fatigue. Patients with chronic abdominal pain may or may not progress to maldigestion, and ~20% of patients will present with symptoms of maldigestion without a history of abdominal pain. Patients with chronic pancreatitis have significant morbidity and mortality and use appreciable amounts of societal resources. Despite steatorrhea, clinically apparent deficiencies of fat-soluble vitamins are surprisingly uncommon. Physical findings in these patients are usually unimpressive, so that there is a disparity between the severity of abdominal pain and the physical signs that usually consist of some mild tenderness. The diagnosis of early or mild chronic pancreatitis can be challenging because there is no biomarker for the disease. Many patients have impaired glucose tolerance with elevated fasting blood glucose levels. The fecal elastase-1 and small-bowel biopsy are useful in the evaluation of patients with suspected pancreatic steatorrhea. The fecal elastase level will be abnormal and small-bowel histology will be normal in such patients. A decrease of fecal elastase level to <100 g per gram of stool strongly suggests severe pancreatic exocrine insufficiency. The radiographic evaluation of a patient with suspected chronic pancreatitis usually proceeds from a noninvasive to more invasive approach. The secretin test becomes abnormal when 60% of the pancreatic exocrine function has been lost. Diffuse calcifications noted on plain film of the abdomen usually indicate significant damage to the pancreas and are pathognomic for chronic pancreatitis. Although alcohol is by far the most common cause of pancreatic calcification, such calcification may also be noted in hereditary pancreatitis, posttraumatic pancreatitis, hypercalcemic pancreatitis, idiopathic chronic pancreatitis, and tropical pancreatitis. Complications of Chronic Pancreatitis the complications of chronic pancreatitis are protean and are listed in Table 371-7. Although most patients have impaired glucose tolerance, diabetic ketoacidosis and diabetic coma are uncommon. Gastrointestinal bleeding may occur from peptic ulceration, gastritis, a pseudocyst eroding into the duodenum, arterial bleeding into the pancreatic duct (hemosuccus pancreaticus), or ruptured varices secondary to splenic vein thrombosis due to chronic inflammation of the tail of the pancreas. Jaundice, cholestasis, and biliary cirrhosis may occur from the chronic inflammatory reaction around the intrapancreatic portion of the common bile duct. Patients with hereditary pancreatitis are at a 10-fold higher risk for pancreatic cancer. Note the markedly dilated pancreatic duct seen in this section through the body and tail (open arrows). Enzyme therapy usually brings diarrhea under control and restores absorption of fat to an acceptable level and affects weight gain. In treating steatorrhea, it is important to use a potent pancreatic formulation that will deliver sufficient lipase into the duodenum to correct maldigestion and decrease steatorrhea. In an attempt to standardize the enzyme activity, potency, and bioavailability, the U. Pharmacopeia Units Product Lipasea Amylasea Immediate-Release Capsule Non-enteric-coated Viokace 10,440 10,440 391,550 Viokace 20,880 20,880 78,300 Delayed-Release Capsules Enteric-coated mini-microspheres Creon 3000 3000 15,000 Creon 6000 6000 30,000 Creon 12,000 12,000 60,000 Creon 24,000 24,000 120,000 Enteric-Coated Mini-Tablets Ultresa 13,800 13,800 27,600 Ultresa 20,700 20,700 41,400 Ultresa 23,000 23,000 46,000 Enteric-Coated Beads Zenpep 3000 3000 16,000 Zenpep 5000 5000 27,000 Zenpep 10,000 10,000 55,000 Zenpep 15,000 15,000 82,000 Zenpep 20,000 20,000 109,000 Zenpep 25,000 25,000 136,000 Enteric-Coated Micro-Tablets Pancreaze 4200 4200 17,500 Pancreaze 10,500 10,500 43,750 Pancreaze 16,800 16,800 70,000 Pancreaze 21,000 21,000 61,000 Bicarbonate-Buffered Enteric-Coated Microspheres Pertzye 8000 8000 30,250 Pertzye 16,000 16,000 60,500 a Proteasea 39,150 78,300 9500 19,000 38,000 76,000 27,600 41,400 46,000 10,000 17,000 34,000 51,000 68,000 85,000 10,000 25,000 40,000 37,000 28,750 57,500 Endoscopic treatment of chronic pancreatitis pain may involve 2101 sphincterotomy, stenting, stone extraction, and drainage of a pancreatic pseudocyst. Therapy directed to the pancreatic duct would seem to be most appropriate in the setting of a dominant stricture, especially if a ductal stone has led to obstruction. The use of endoscopic stenting for patients with chronic pain, but without a dominant stricture, has not been subjected to any controlled trials. In patients with large-duct disease usually from alcohol-induced chronic pancreatitis, ductal decompression with surgical therapy has been the therapy of choice. Among such patients, 80% seem to obtain immediate relief; however, at the end of 3 years, one-half of the patients have recurrence of pain. This would suggest that chronic pancreatitis patients with dilated ducts and pain should be considered for surgical intervention. A Whipple procedure, total pancreatectomy, and autologous islet cell transplantation have been used in selected patients with chronic pancreatitis and abdominal pain refractory to conventional therapy. The patients who have benefited the most from total pancreatectomy have chronic pancreatitis without prior pancreatic surgery or evidence of islet cell insufficiency. Recent meta-analyses have shown no consistent benefit of enzyme therapy at reducing pain in chronic pancreatitis. In some patients with idiopathic chronic pancreatitis, conventional nonenteric-coated enzyme preparations containing high concentrations of serine proteases may relieve mild abdominal pain or discomfort. It is important to recognize and treat with prokinetic drugs because treatment with enzymes may fail simply because gastric dysmotility is interfering with the delivery of enzymes into the upper intestine. A recent prospective study reported that pregabalin can improve pain in chronic pancreatitis and lower pain medication requirement. The codon 122 mutations lead to a substitution of the corresponding arginine with another amino acid, usually histidine. This substitution, when it occurs, eliminates a fail-safe trypsin self-destruction site necessary to eliminate trypsin that is prematurely activated within the acinar cell. These patients have recurring attacks of severe abdominal pain that may last from a few days to a few weeks. A recent natural history study of hereditary pancreatitis in more than 200 patients from France reported that abdominal pain started in childhood at age 10 years, steatorrhea developed at age 29 years, diabetes at age 38 years, and pancreatic carcinoma at age 55 years. Such an annular pancreas may cause intestinal obstruction in the neonate or the adult. Symptoms of postprandial fullness, epigastric pain, nausea, and vomiting may be present for years before the diagnosis is entertained. The radiographic findings are symmetric dilation of the proximal duodenum with bulging of the recesses on either side of the annular band, effacement but not destruction of the duodenal mucosa, accentuation of the findings in the right anterior oblique position, and lack of change on repeated examinations. Pancreas divisum is the most common congenital anatomic variant of the human pancreas. Current evidence indicates that this anomaly does not predispose to the development of pancreatitis in the great majority of patients who harbor it. However, the combination of pancreas divisum and a small accessory orifice could result in dorsal duct obstruction. In many of these patients, pancreatitis is idiopathic and unrelated to the pancreas divisum. Patients with this condition demonstrate an elevated serum amylase value and a low urinary amylase value. Immature dendritic cells,ordendriticcellprecursors,arekeycomponentsoftheinnate immune system by responding to infections with production of high levels of cytokines. Additional cells of the adaptive immune system include various types of antigenpresentingcells. From invertebrates, humans have inherited the innate immune system, an ancient defense system that uses germline-encoded proteins to recognize pathogens. Anappreciation of the cellular and molecular bases of innate and adaptive immune responses is critical to understanding the pathogenesis of inflammatory,autoimmune,infectious,andimmunodeficiencydiseases. New York: Garland Publishing, 1997; R Brines et al: Immunology Today 18S:1, 1997; and S Shaw (ed): Protein reviews on the Web. Tissue macrophages arise from monocytes that have migrated out of the circulation and by in situ proliferation of macrophage precursors in tissue. Inflammatory mediators produced by macrophages attract additional effector cells such as neutrophils to the site of infection. Monocytesmacrophages mediate innate immune effector functions such as destructionofantibody-coatedbacteria,tumorcells,orevennormal hematopoietic cells in certain types of autoimmune cytopenias. Neutrophils, Eosinophils, and Basophils Granulocytes are present in nearly all forms of inflammation and are amplifiers and effectors of innate immune responses. This is a particularly important host defense mechanism against parasitic diseases. The three pathways of compleIn this figure, the arrows denote that cells develop from precursor cells or produce cytokines or antiment activation all converge on the bodies; lines ending with bars indicate suppressive intercellular interactions. C3 into either T cells, antigen-presenting dendritic cells, natural killer cells, macrophages, granulocytes, cleavage by each pathway results in or B cells. They are critical for both normal innate and adaptive immune responses, and their expression may be perturbedinmostimmune,inflammatory,andinfectiousdiseasestates. Ingeneral,cytokinesarecharacterizedby considerable redundancy; different cytokines have similar functions. Cytokines have been named based on presumed targets or based on presumed functions. Many cytokines that were originally described as having a certain function have retained those names. In this regard, cytokines can have dramatic effects on the regulation of immune responses and the pathogenesis of a variety of diseases. The immunoglobulin (Ig) superfamily represents a large number of cell-surface and secreted proteins. The hallmark of the hematopoietic growth factor (type 1) receptor family is that the extracellular regions of each receptor contain two conservedmotifs. A key feature of adaptive immunity is that following the initial contact with antigen (immunologic priming), subsequent antigen exposure leads to more rapid and vigorous immune responses (immunologic memory). The proportion and distribution of immunocompetent cells in various tissues reflect cell traffic, homing patterns, and functional capabilities. Thus,thespecificcytokine receptor is responsible for ligand-specific binding, whereas the subunitssuchasgp130,the150-kDasubunit,andcareimportantin signaltransduction. Significant advances have been made in defining the signaling pathways through which cytokines exert their intracellular effects. Elements of the developing T and B cell receptor for antigen are shown schematically. The classification into the various stages of B cell development is primarily defined by rearrangement of the immunoglobulin (Ig) heavy (H) and light (L) chain genes and by the absence or presence of specific surface markers. Antigens taken up from the extracellular space via endocytosis into intracellular acidified vesicles are degraded by vesicle proteases intopeptidefragments. Each of the pathways results in the activation of particular transcription factors that control the expression of cytokine andcytokinereceptorgenes. T cell superantigens include staphylococcal enterotoxins and otherbacterialproducts. B lymphocyte development can be separated into antigenindependent and antigen-dependent phases. Antigendependent B cell maturation is driven by the interaction of antigen with the mature B cell sIg, leading to memory B cell induction, Ig classswitching,andplasmacellformation. The process of Ig gene rearrangement is regulated and results in a single antibody specificity produced by each B cell, with each Ig molecule comprising one type of heavy chain and one type of light chain. This overall process of generating the best antibodies is calledaffinity maturation of antibody. Lymphocytes that synthesize IgG, IgA, and IgE are derived from sIgM+, sIgD+ mature B cells. Ig class switching occurs in lymph node and other peripheral lymphoid tissue germinal centers. Thefour IgG subclasses are numbered in order of their level in serum, IgG1 being found in greatest amounts and IgG4 the least. IgG antibodies are frequently the predominant antibody made after rechallenge of the host with antigen (secondary antibodyresponse). IgM is the first immunoglobulin to appear in the immuneresponse(primaryantibodyresponse)andistheinitialtype ofantibodymadebyneonates. MembraneIgMinthemonomericform also functions as a major antigen receptor on the surface of mature B cells (Table 372e-12). For example, IgM antibodies againstIgGmolecules(rheumatoidfactors)arepresentinhightiters in rheumatoid arthritis, other collagen diseases, and some infectious diseases(subacute bacterial endocarditis).
Biopsies from the ulcer bases have the greatest diagnostic yield for finding the pathognomonic large nuclear or cytoplasmic inclusion bodies discount erectile dysfunction pills purchase 20mg cialis super active. Valganciclovir (900 mg two times a day) zinc causes erectile dysfunction cheap cialis super active express, an oral formulation of ganciclovir best pills for erectile dysfunction yahoo buy cheap cialis super active 20mg online, can also be used erectile dysfunction treatment prostate cancer buy cialis super active canada. Esophageal perforation is confirmed by a contrast swallow erectile dysfunction nclex questions 20mg cialis super active with mastercard, usually Gastrografin followed by thin barium erectile dysfunction middle age discount cialis super active 20 mg without a prescription. Endoscopic clipping or stent placement may be indicated in nonoperated iatrogenic perforations or nonoperable cases such as perforated tumors. Bleeding usually abates spontaneously, but protracted bleeding may respond to local epinephrine or cauterization therapy, endoscopic clipping, or angiographic embolization. Radiation exposure in excess of 5000 cGy has been associated with increased risk of esophageal stricture. Severe corrosive injury may lead to esophageal perforation, bleeding, stricture, and death. Generally, this is attributed to poor "pill taking habits": inadequate liquid with the pill or lying down immediately after taking a pill. Since initially reported in 1970, more than 1000 cases of pill esophagitis have been reported, suggesting that this is not an unusual occurrence. Typical symptoms of pill esophagitis are the sudden onset of chest pain and odynophagia. Instrument perforation from endoscopy or nasogastric tube placement typically occurs in the hypopharynx or at the gastroesophageal junction. Perforation may also occur at the site of a stricture in the setting of endoscopic food disimpaction or esophageal dilation. Food impaction may occur due to stricture, carcinoma, Schatzki ring, eosinophilic esophagitis, or simply inattentive eating. If it does not spontaneously resolve, impacted food can be dislodged endoscopically. After emergent treatment, patients should be evaluated for potential causes of the impaction with treatment rendered as indicated. The financial impact of these common disorders has been substantial, with an estimated burden on direct and indirect health care costs of ~$6 billion per year in the United States, with $3 billion spent on hospitalizations, $2 billion on physician office visits, and $1 billion in decreased productivity and days lost from work. Gastric Anatomy the gastric epithelial lining consists of rugae that contain microscopic gastric pits, each branching into four or five gastric glands made up of highly specialized epithelial cells. The parietal cell, also known as the oxyntic cell, is usually found in the neck, or isthmus, or in the oxyntic gland. The resting, or unstimulated, parietal cell has prominent cytoplasmic tubulovesicles and intracellular canaliculi containing short microvilli along its apical surface. However, this nomenclature subsequently proved unfortunate and has been discarded because an estimated half of qualifying patients do not have an identifiable systemic disease, and reflux disease is often the only identifiable association. When scleroderma esophagus occurs as a manifestation of a collagen vascular disease, the histopathologic findings are of infiltration and destruction of the esophageal muscularis propria with collagen deposition and fibrosis. Dysphagia may also be manifest but is generally mild and alleviated by eating in an upright position and using liquids to facilitate solid emptying. Erosive lichen planus, Stevens-Johnson syndrome, and graft-versus-host disease can also involve the esophagus. An ulcer is defined as disruption of the mucosal integrity of the stomach and/or duodenum leading to a local defect or excavation due to active inflammation. In addition, a steady flow of exogenous substances such as medications, alcohol, and bacteria encounter the gastric mucosa. The first line of defense is a mucus-bicarbonatephospholipid layer, which serves as a physicochemical barrier to multiple molecules, including hydrogen ions. Mucus is secreted in a regulated fashion by gastroduodenal surface epithelial cells. It consists primarily of water (95%) and a mixture of phospholipids and glycoproteins (mucin). The mucous gel functions as a nonstirred water layer impeding diffusion of ions and molecules such as pepsin. Bicarbonate, secreted in a regulated manner by surface epithelial cells of the gastroduodenal mucosa into the mucous gel, forms a pH gradient ranging from 1 to 2 at the gastric luminal surface and reaching 6 to 7 along the epithelial cell surface. Surface epithelial cells provide the next line of defense through several factors, including mucus production, epithelial cell ionic transporters that maintain intracellular pH and bicarbonate production, and intracellular tight junctions. Surface epithelial cells generate heat shock proteins that prevent protein denaturation and protect cells from certain factors such as increased temperature, cytotoxic agents, or oxidative stress. Epithelial cells also generate trefoil factor family peptides and cathelicidins, which also play a role in surface cell protection and regeneration. This process occurs independent of cell division and requires uninterrupted blood flow and an alkaline pH in the surrounding environment. In tandem with epithelial cell renewal, formation of new vessels (angiogenesis) within the injured microvascular bed occurs. Moreover, this microcirculatory bed provides an adequate supply of micronutrients and oxygen while removing toxic metabolic by-products. The gastric mucosa contains abundant levels of prostaglandins that regulate the release of mucosal bicarbonate and mucus, inhibit parietal cell secretion, and are important in maintaining mucosal blood flow and epithelial cell restitution. Prostaglandins are derived from esterified arachidonic acid, which is formed from phospholipids (cell membrane) by the action of phospholipase A2. Physiology of Gastric Secretion Hydrochloric acid and pepsinogen are the two principal gastric secretory products capable of inducing mucosal injury. Gastric acid and pepsinogen play a physiologic role in protein digestion; absorption of iron, calcium, magnesium, and vitamin B12; and killing ingested bacteria. Basal acid production occurs in a circadian pattern, with highest levels occurring during the night and lowest levels during the morning hours. Cholinergic input via the vagus nerve and histaminergic input from local gastric sources are the principal contributors to basal acid secretion. The last phase of gastric acid secretion is initiated as food enters the intestine and is mediated by luminal distention and nutrient assimilation. A series of pathways that inhibit gastric acid production are also set into motion during these phases. The parietal cell expresses receptors for several stimulants of acid secretion, including histamine (H2), gastrin (cholecystokinin B/gastrin receptor), and acetylcholine (muscarinic, M3). Histamine also stimulates gastric acid secretion indirectly by activating the histamine H3 receptor on D-cells, which inhibits somatostatin release. The active catalytic site is found within the subunit; the function of the subunit is unclear. Ulcers are defined as breaks in the mucosal surface >5 mm in size, with depth to the submucosa. The mechanisms by which some of these risk factors lead to ulcer disease are highlighted below. The tubulovesicles are impermeable to K+, which leads to an inactive pump in this location. Proton pumps are recycled back to the inactive state in cytoplasmic vesicles once parietal cell activation ceases. In addition, acid secretion requires a number of apical and basolateral parietal cell membrane chloride and potassium channels. The chief cell, found primarily in the gastric fundus, synthesizes and secretes pepsinogen, the inactive precursor of the proteolytic enzyme pepsin. It may attach to gastric epithelium but under normal circumstances does not appear to invade cells. It is strategically designed to live within the aggressive environment of the stomach. The organism is capable of transforming into a coccoid form, which represents a dormant state that may facilitate survival in adverse conditions. Once in the cell, Cag A activates a series of cellular events important in cell growth and cytokine production. Urease produces ammonia from urea, an essential 1915 step in alkalinizing the surrounding pH. Additional bacterial factors include catalase, lipase, adhesins, platelet-activating factor, and pic B (induces cytokines). Moreover, with the present rate of intervention, the organism will be ultimately eliminated from the United States. The rate of infection in the United States has fallen by >50% when compared to 30 years ago. The basis for this difference is unknown, but is likely due to a combination of host and bacterial factors some of which are outlined below. These virulence factors, in conjunction with additional bacterial constituents, can cause mucosal damage, in part through their ability to target the host immune cells. The bacteria produce surface factors that are chemotactic for neutrophils and monocytes, which in turn contribute to epithelial cell injury (see below). Host factors: Studies in twins suggest that there may be genetic predisposition to acquire H. Finally, the human stomach can be colonized by a host of commensal organisms that may affect the likelihood of H. The type and distribution of gastritis correlate with the ultimate gastric and duodenal pathology observed. More than 30 billion over-thecounter tablets and over 100 million prescriptions are sold yearly in the United States alone. It therefore follows that interruption of prostaglandin synthesis can impair mucosal defense and repair, thus facilitating mucosal injury via a systemic mechanism. Moreover, enteric-coated or buffered preparations are also associated with risk of peptic ulceration. Not only have smokers been found to have ulcers more frequently than do nonsmokers, but smoking appears to decrease healing rates, impair response to therapy, and increase ulcer-related complications such as perforation. Theories have included altered gastric emptying, decreased proximal duodenal bicarbonate production, increased risk for H. Increased frequencies of blood group O and of the nonsecretor status have also been implicated as genetic risk factors for peptic diathesis. Certain foods and beverages can cause dyspepsia, but no convincing studies indicate an association between ulcer formation and a specific diet. Disorders with a possible association are (1) hyperparathyroidism, (2) coronary artery disease, (3) polycythemia vera, (4) chronic pancreatitis, (5) former alcohol use, (6) obesity, (7) African-American race, and (8) three or more doctor visits in a year. Physical examination is critically important for discovering evidence of ulcer complication. Presence of a succussion splash indicates retained fluid in the stomach, suggesting gastric outlet obstruction. Bleeding and complications of ulcer disease occur more often in individuals >60 years of age. Up to 20% of patients with ulcer-related hemorrhage bleed without any preceding warning signs or symptoms. Penetration is a form of perforation in which the ulcer bed tunnels into an adjacent organ. A patient may have relative obstruction secondary to ulcer-related inflammation and edema in the peripyloric region. A fixed, mechanical obstruction secondary to scar formation in the peripyloric areas is also possible. Up to 60% of patients seeking medical care for dyspepsia have a negative diagnostic evaluation. Despite this poor correlation, a careful history and physical examination are essential components of the approach to a patient suspected of having peptic ulcers. The discomfort is also described as an ill-defined, aching sensation or as hunger pain. Several possible explanations include acidinduced activation of chemical receptors in the duodenum, enhanced duodenal sensitivity to bile acids and pepsin, or altered gastroduodenal motility. A urinary Hp antigen test, as well as a ulcer requires either a radiographic (barium study) or an endoscopic refined monoclonal antibody stool antigen test, appears promising. A summary of commonly used drugs for mucosal folds originating from the ulcer margin. Endoscopic examination is particularly helpful in identifying lesions too small to detect by radiographic examination, for evaluation of atypical radiographic abnormalities, or to determine if an ulcer is a source of blood loss. The most commonly used agents are mixtures of aluminum hydroxide and magnesium hydroxide. Aluminum hydroxide can produce constipation and phosphate depletion; magnesium hydroxide may cause loose stools.


















