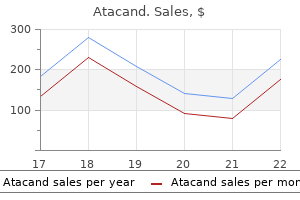
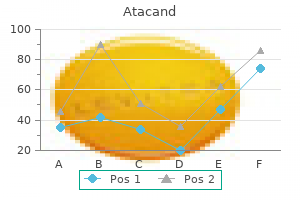
Atacand

Michael D. Burg, MD, FACEP
- Assistant Clinical Professor
- Department of Emergency Medicine
- Medical Education Program
- University of California, San Francisco-Fresno
- Fresno, California
Initial medical treatment of acute pancreatitis: American gastroenterological association institute technical review symptoms of hiv infection buy atacand 16 mg without a prescription. American Gastroenterological Association Institute guideline on initial management of acute pancreatitis antiviral elixir order 4 mg atacand. Early versus delayed feeding in patients with acute pancreatitis: a systematic review hiv symptoms time frame infection order atacand 16mg on-line. Pseudocyst drainage predisposes to infection when pancreatic necrosis is unrecognized hiv infection menstrual cycle buy atacand 16 mg mastercard. Pancreatic pseudocysts following acute pancreatitis: risk factors influencing therapeutic outcomes hiv infection mouth ulcers purchase 4 mg atacand with amex. Treatment of pancreatic pseudocysts antiviral used to treat flu buy discount atacand 16mg online, pancreatic necrosis, and pancreatic duct leaks. Endoscopic transmural drainage of peripancreatic fluid collections: outcomes and predictors of treatment success in 211 consecutive patients. Predictors of outcome in pancreatic duct disruption managed by endoscopic transpapillary stent placement. Endoscopic ultrasound drainage of pancreatic pseudocyst: a prospective comparison with conventional endoscopic drainage. Endoscopic drainage of pancreatic-fluid collections in 116 patients: a comparison of etiologies, drainage techniques, and outcomes. Endoscopic ultrasound-guided versus conventional transmural drainage for pancreatic pseudocysts: a prospective randomized trial. Endoscopic therapy for sphincter of Oddi dysfunction in idiopathic pancreatitis: from empiric to scientific. Similar efficacies of biliary, with or without pancreatic, sphincterotomy in treatment of idiopathic recurrent acute pancreatitis. Sensitivity of endoscopic ultrasound, multidetector computed tomography, and magnetic resonance cholangiopancreatography in the diagnosis of pancreas divisum: a tertiary center experience. Clinical outcomes in patients who undergo extracorporeal shock wave lithotripsy for chronic calcific pancreatitis. Treatment for painful calcified chronic pancreatitis: extracorporeal shock wave lithotripsy versus endoscopic treatment: a randomised controlled trial. Extracorporeal shock wave lithotripsy in the management of chronic calcific pancreatitis: a meta-analysis. Endoscopic treatment of pancreatic duct stones under direct vision: revolution or resignation Endoscopic treatment of chronic pancreatitis: a multicenter study of 1000 patients with long-term follow-up. Wire-guided pancreatic pseudocyst drainage by using a modified needle knife and therapeutic echoendoscope. Endoscopic drainage of pancreatic pseudocysts: long-term outcome and procedural factors associated with safe and successful treatment. Endoscopic ultrasoundguided drainage of pancreatic fluid collections with indeterminate adherence using temporary covered metal stents. Single-step endoscopic ultrasonography-guided drainage of peripancreatic fluid collections with a single self-expandable metal stent and standard linear echoendoscope. Primary and overall success rates for clinical outcomes after laparoscopic, endoscopic, and open pancreatic cystogastrostomy for pancreatic pseudocysts. The revised Atlanta classification for acute pancreatitis: updates in imaging terminology and guidelines. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Percutaneous transgastric irrigation drainage in combination with endoscopic necrosectomy in necrotizing pancreatitis (with videos). Aggressive endoscopic therapy for pancreatic necrosis and pancreatic abscess: a new safe and effective treatment algorithm (videos). A comparison of direct endoscopic necrosectomy with transmural endoscopic drainage for the treatment of walled off pancreatic necrosis. A multi-institutional consensus on how to perform endoscopic ultrasound-guided peri-pancreatic fluid collection drainage and endoscopic necrosectomy. Endoscopic management of acute necrotizing pancreatitis: European Society of Gas- 69. Endoscopic ultrasonographyguided pancreatic duct access: techniques and literature review of pancreatography, transmural drainage and rendezvous techniques. A unifying concept: pancreatic ductal anatomy both predicts and determines the major complications resulting from pancreatitis. Temporary placement of covered self-expandable metal stents in benign biliary strictures: a new paradigm Efficacy of self-expandable metal stents in management of benign biliary strictures and comparison with multiple plastic stents: a meta-analysis. Endoscopic therapy with multiple plastic stents for benign biliary strictures due to chronic calcific pancreatitis: the good, the bad, and the ugly. Endoscopic transpapillary drainage for external fistulas developing after surgical or radiological pancreatic interventions. Pancreatic stent placement is associated with resolution of refractory grade C pancreatic fistula after left-sided pancreatectomy. Endoscopic treatment as first-line therapy for pancreatic ascites and pleural effusion. Endoscopic transpapillary stenting or conservative treatment for pancreatic fistulas in necrotizing pancreatitis: multicenter series and literature review. Endoscopic sealing of pancreatic fistulas: Four case reports and review of the literature. Advances in gastrointestinal interventions: the treatment of gastroduodenal and colorectal obstructions with metallic stent. Role of self-expandable metal stents in the palliation of malignant duodenal obstruction. Combined endoscopic stent insertion in malignant biliary and duodenal obstruction. Management of simultaneous biliary and duodenal obstruction: the endoscopic perspective. American gastroenterological association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. The liver diverticulum forms through the proliferation of endodermal cells at the cranioventral junction of the yolk sac with the foregut and grows into the septum transversum in a cranioventral direction. At the 5-mm stage, a solid cranial portion (hepatic) and a hollow caudal portion of the diverticulum can be clearly distinguished. The large hepatic portion differentiates into proliferating cords of hepatocytes and the intrahepatic bile ducts. Its expression disappears as soon as hepatoblasts invade the septum transversum but reappears in cells of the biliary lineage throughout the development. The homeobox gene Hhex is essential for proper hepatoblast differentiation and bile duct morphogenesis. At the 3- to 4-mm stage, between the third and fourth weeks of gestation, the growing diverticulum projects as an epithelial plug into the septum transversum. In this chapter, the embryologic and anatomic characteristics of the bile ducts and gallbladder are reviewed, with a focus on information useful for diagnosing and treating biliary tract disease and understanding the anomalies and congenital malformations of these structures. Biliary tract disease in infants and children is considered because many of the disorders that occur early in life are due to abnormal morphogenesis or adversely affect the process of development. A second layer of primitive hepatocytes is similarly transformed and produces a circular cleft around the portal vein that is lined on both sides by bile duct epithelial cells. Thus the entire network of interlobular and intralobular bile ductules develops from the limiting plate. Bile ducts develop according to 2 axes: ducts mature along their radial axis, and they also grow in length according to an axis that extends from the hilum of the liver to the periphery of the liver lobes. In sections of the 10-mm embryo, many of the liver cords are traversed by double-walled canals that branch and are morphologically indistinguishable from bile capillaries of the adult. These structures differ from those of the adult in that they are bounded by 6 or more liver cells instead of 2. The process of differentiation of bile ductular epithelial cells (cholangiocytes) from primitive hepatocytes has been documented in humans using immunohistochemical staining with several anticytokeratin antibodies. During the transition from ductal plates to bile ducts, portal myofibroblasts expand significantly and surround newly formed bile ducts. Periportal connective tissue, corticosteroid hormones, and basal laminar components may play important roles in the differentiation of bile ducts. The ductal plate structure requires extensive remodeling through a process of reabsorption, possibly through apoptosis, to yield the characteristic anastomosing system of biliary channels that surround the portal vein. Proteins that appear to have a role in the promotion of apoptosis, specifically Fas antigen and c-Myc, are consistently detected in primitive intrahepatic ductal cells. Bcl-2 protein, an inhibitor of apoptosis, is not found in early stages of intrahepatic bile duct cell development but becomes detectable later. Development of the extrahepatic biliary system precedes that of intrahepatic bile ducts. The extrahepatic system (but not intrahepatic bile ducts) are derived from a progenitor cell expressing the transcription factor pancreatic-duodenal homeobox 1 (Pdx1). Appropriate segregation of extrahepatic biliary system and ventral pancreatic lineages is also regulated by hairy and enhancer of split-1 (Hes1), a transcriptional effector of Notch signaling. At 16 mm, the cystic duct and proximal gallbladder are hollow, but the fundus of the gallbladder is still partially obstructed by remnants of the epithelial plug. The characteristic folds of the gallbladder are formed toward the end of gestation and are moderately developed in the neonate. Bile secretion starts at the beginning of the fourth month of gestation; thereafter, the biliary system continuously contains bile, which is secreted into the gut and imparts a dark green color to the intestinal contents (meconium). The duct is lined by a layer of cuboidal epithelial cells that are joined by tight junctions (long arrow) and demonstrate a microvillar architecture on their luminal surface (short arrow). Quantitative computer-aided 3D imaging has estimated the volume of the entire macroscopic duct system of human liver to be a mean of 20. These structures are far from being inert channels; they are capable of modifying biliary flow and composition significantly in response to hormones such as secretin. No major ultrastructural differences exist between cholangiocytes lining small and large bile ducts, but the functional properties of cholangiocytes are heterogeneous. The canaliculi form a meshwork of polygonal channels between hepatocytes with many anastomotic interconnections. At the most proximal level, one or more fusiform-shaped ductular cells may share a canalicular lumen with a hepatocyte; gradually, the ductules become lined by 2 to 4 cuboidal epithelial cells as they approach the portal canal. The terminal bile ductules are thought to proliferate as a result of chronic extrahepatic bile duct obstruction. The muscular component may provide the morphologic basis for the narrowing of the ducts at this level, as observed on cholangiography. These ducts anastomose further to form the large hilar intrahepatic ducts, which are 1 to 1. The common hepatic duct emerges from the porta hepatis after the union of the right and left hepatic ducts, each of which is 0. This sheath of fibrous tissue binds the hepatic ducts to the adjacent blood vessels. In the adult, the common hepatic duct is about 3 cm long and is joined by the cystic duct, usually at its right side, to form the common bile duct (or simply bile duct). The cystic duct enters the common hepatic duct directly in 70% of patients; alternatively, the cystic duct may run anterior or posterior to the bile duct and spiral around it before joining the bile duct on its medial side. Many side branches end as blind pouches, but others, particularly at the hilum, communicate with each other. At the bifurcation, side branches from several main bile ducts connect to form a plexus. The blind pouches may serve to store or modify bile, whereas the biliary plexus provides anastomoses that may allow exchange of material between the large bile ducts. The anatomy of the hepatic hilum is particularly important to the surgeon (see also Chapter 71). A plate of fibrous connective tissue in the hepatic hilum includes the umbilical plate that envelops the umbilical portion of the portal vein, the cystic plate in the gallbladder bed, and the Arantian plate that covers the ligamentum venosum. The bile ducts in the plate system correspond to the extrahepatic bile ducts, and their lengths are variable in every segment. Mucus-secreting tubular glands can be found at regular intervals in the submucosa, with openings to the surface of the mucosa. The smooth muscle component is conspicuous only at the neck of the gallbladder and at the lower end of the bile duct. The bile duct passes retroperitoneally behind the first portion of the duodenum in a notch on the back of the head of the pancreas and enters the second part of the duodenum. The duct then passes obliquely through the posterior medial aspect of the duodenal wall and joins the main pancreatic duct to form the ampulla of Vater In 10% to 15% of patients, the bile and pancreatic ducts open separately into the duodenum. Contraction of the fasciculi longitudinales shortens the length of the bile duct and, thus, promotes the flow of bile into the duodenum. The contraction of the sphincter ampullae shortens the ampulla and approximates the ampullary folds to prevent reflux of intestinal contents into the bile and pancreatic ducts. When both ducts end in the ampulla, however, contraction of the sphincter may cause reflux of bile into the pancreatic duct. An abundant anastomotic network of blood vessels from branches of the hepatic and gastroduodenal arteries supplies the bile duct. An extraordinarily rich plexus of capillaries surrounds bile ducts as they pass through the portal tracts. The peribiliary plexus may modify biliary secretions through the bidirectional exchange of proteins, inorganic ions, and bile acids between blood and bile. Because blood flows in the direction (from the large toward the small ducts) opposite to that of bile flow, the peribiliary plexus presents a countercurrent stream of biliaryreabsorbed substances to hepatocytes. The intrahepatic arteries, veins, bile ducts, and hepatocytes are innervated by adrenergic and cholinergic nerves. In the autonomic nervous system, there are a number of regulatory peptides, such as neuropeptide tyrosine, calcitonin gene-related peptide, somatostatin, vasoactive intestinal polypeptide, enkephalin, and bombesin. Neuropeptide tyrosine-positive nerves present in extrahepatic bile ducts may serve to regulate bile flow by autocrine or paracrine mechanisms.
Diseases
- X chromosome, trisomy Xp3
- Lichen spinulosus
- Situs inversus totalis with cystic dysplasia of kidneys and pancreas
- Anophthalmos, clinical
- Female sexual arousal disorder
- Osteochondritis deformans juvenile
- Acute myeloblastic leukemia type 6
- Trisomy 11 mosaicism
- Hyperparathyroidism, neonatal severe primary
- Enuresis
Stones are then fragmented using a variety of techniques anti virus warning mac purchase atacand 4 mg on-line, with a high rate of success (see Chapter 66) hiv infection globally atacand 4 mg lowest price. Bleeding hiv infection prevention buy cheapest atacand, which occurs with such aggressive dilation hiv infection rate in new york cheap atacand, often requires maintenance of an external catheter to drain blood within the biliary tract hiv aids infection rates uk order atacand in united states online. Patients with intrahepatic gallbladders and small main symptoms hiv infection discount 8mg atacand otc, shrunken, thick-walled gallbladders are not candidates for this approach. A Murphy sign can be difficult, if not impossible, to demonstrate, particularly in an intubated or unresponsive patient. Delayed diagnosis and treatment can lead to gallbladder gangrene and perforation and to mortality. In patients in whom the clinical suspicion for acute acalculous cholecystitis is high, a gallbladder tube should be placed percutaneously. In one study of 55 critically ill patients with suspected acute acalculous cholecystitis who underwent percutaneous gallbladder tube placement, clinical improvement was seen in 58. The guidewire is passed into the duodenum and identified endoscopically (inset), after which it is grasped with a snare and pulled through the endoscope and out through the mouth, thereby providing access to the biliary tract. Endoscopic ultrasound-guided biliary drainage: a systematic review and meta-analysis. Prospective international multicenter study on endoscopic ultrasound-guided biliary drainage for patients with malignant distal biliary obstruction after failed endoscopic retrograde cholangiopancreatography. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopic ultrasound rendezvous for bile duct access using a transduodenal approach: cumulative experience at a single center. Ultrasound evaluation of gallbladder dyskinesia: comparison of scintigraphy and dynamic 3D and 4D ultrasound techniques. Evaluation of gallbladder and biliary duct disease using microbubble contrast-enhanced ultrasound. Endoscopic ultrasound versus magnetic resonance cholangiopancreatography for common bile duct stones. Patient characteristics and risk factors for nephrogenic systemic fibrosis following gadolinium exposure. Multidetector computed tomography cholangiography with multiplanar reformation for the assessment of patients with biliary obstruction. Suspected choledocholithiasis: endoscopic ultrasound or magnetic resonance cholangio-pancreatography Magnetic resonance cholangiopancreatography in the diagnosis of primary sclerosing cholangitis. Endoscopic balloon sphincter dilation (sphincteroplasty) versus sphincterotomy for common bile duct stones. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Transpapillary cholangioscopy-directed lithotripsy in patients with difficult bile duct stones. Endoscopic papillary large-balloon dilation combined with endoscopic biliary sphincterotomy for the removal of bile duct stones (with video). Combination of endoprostheses and oral ursodeoxycholic acid or placebo in the treatment of difficult to extract common bile duct stones. Use of covered self-expandable metal stents for endoscopic management of benign biliary disease not related to stricture (with video). Endoscopic treatment of nonstricture-related benign biliary diseases using covered self-expandable metal stents. A twenty-year experience with endoscopic therapy for symptomatic primary sclerosing cholangitis. Screening and diagnosis of cholangiocarcinoma in patients with primary sclerosing cholangitis. Long-term outcomes of positive fluorescence in situ hybridization tests in primary sclerosing cholangitis. Cholangioscopic characterization of dominant bile duct stenoses in patients with primary sclerosing cholangitis. Refined probe-based confocal laser endomicroscopy classification for biliary strictures: the Paris Classification. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Multiple stenting of refractory pancreatic duct strictures in severe chronic pancreatitis: long-term results. Fully covered self-expandable metal stents in biliary strictures caused by chronic pancreatitis not responding to plastic stenting: a prospective study with 2 years of follow-up. Self-expanding metal stents for preoperative biliary drainage in patients receiving neoadjuvant therapy for pancreatic cancer. Biliary self-expandable metal stents do not adversely affect pancreaticoduodenectomy. Metal or plastic stents for preoperative biliary drainage in resectable pancreatic cancer. Biliary stenting versus bypass surgery for the palliation of malignant distal bile duct obstruction: a meta-analysis. Malignant distal biliary obstruction: a systematic review and meta-analysis of endoscopic and surgical bypass results. Cost efficacy of metal stents for palliation of extrahepatic bile duct obstruction in a randomized controlled trial. Understanding risk factors and avoiding complications with endoscopic retrograde cholangiopancreatography. Rectal nonsteroidal anti-inflammatory drugs are superior to pancreatic duct stents in preventing pancreatitis after endoscopic retrograde cholangiopancreatography: a network meta-analysis. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. A comprehensive approach to the management of acute endoscopic perforations (with videos). Case volume and outcome of endoscopic retrograde cholangiopancreatography: results results of a nationwide Austrian benchmarking project. Meta-analysis of randomized trials comparing the patency of covered and uncovered selfexpandable metal stents for palliation of distal malignant bile duct obstruction. The management of highgrade hilar strictures by endoscopic insertion of self-expanding metal endoprostheses. Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. Endoscopic stenting for hilar cholangiocarcinoma: efficacy of unilateral and bilateral placement of plastic and metal stents in a retrospective review of 480 patients. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. Factors associated with increased survival after photodynamic therapy for cholangiocarcinoma. Unresectable cholangiocarcinoma: comparison of survival in biliary stenting alone versus stenting with photodynamic therapy. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Endoscopic radiofrequency ablation for malignant biliary obstruction: a nationwide 120. Sedations and analgesia in patients undergoing percutaneous transhepatic biliary drainage. Ultrasound and fluoroscopy guided percutaneous transhepatic biliary drainage in patients with nondilated bile ducts. Hepatic arterial injuries after percutaneous biliary interventions in the era of laparoscopic surgery and liver transplantation: experience with 930 patients. Percutaneous transhepatic treatment of hepaticojejunal anastomotic biliary strictures after living donor liver transplantation. Percutaneous management of biliary strictures after pediatric liver transplantation. Long-term follow-up of percutaneous transhepatic balloon cholangioplasty in the management of biliary strictures after liver transplantation. Percutaneous transhepatic biliary drainage may serve as a successful rescue procedure in failed cases of endoscopic therapy for a post-living donor liver transplantation biliary stricture. Safety and efficacy of the percutaneous treatment of bile leaks in hepaticojejunostomy or split-liver transplantation without dilatation of the biliary tree. Percutaneous management of anastomotic bile leaks following liver transplantation. Percutaneous transhepatic cholangiodrainage as rescue therapy for symptomatic biliary leakage without biliary tract dilation after major surgery. Biliary tract complications after orthotopic liver transplantation with choledochocholedochostomy anastomosis: endoscopic endoscopic findings and results of therapy. Endoscopic diagnosis and treatment of biliary leak in patients following liver transplantation: a prospective clinical study. Results of endoscopic retrograde cholangiopancreatography in the treatment of biliary tract complications after orthotopic liver transplantation: our experience. Endoscopic management is the treatment of choice for bile leaks after liver resection. Elevated stricture rate following the use of fully covered self-expandable metal biliary stents for biliary leaks following liver transplantation. Efficacy and safety of fully covered self-expandable metallic stents in biliary complications after liver transplantation: a preliminary study. Postsurgical bile leaks: endoscopic endoscopic obliteration of the transpapillary pressure gradient is enough. Management of iatrogenic bile duct injuries: role role of the interventional radiologist. Percutaneous management of bile duct strictures and injuries associated with laparoscopic cholecystectomy: a decade of experience. Percutaneous treatment of biliary stones: sphincteroplasty sphincteroplasty and occlusion balloon for the clearance of bile duct calculi. Percutaneous treatment of extrahepatic bile duct stones assisted by balloon sphincteroplasty and occlusion balloon. Percutaneous video choledochoscopic treatment of retained biliary stones via dilated T-tube tract. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Preoperative biliary drainage in perihilar cholangiocarcinoma: identifying patients who require percutaneous drainage after failed endoscopic drainage. Common bile duct obstruction due to malignancy: treatment with plastic versus metal stents. One-step palliative treatment method for obstructive jaundice caused by unresectable malignancies by percutaneous transhepatic insertion of an expandable metallic stent. Endoscopic or percutaneous biliary drainage for gallbladder cancer: a randomized trial and quality of life assessment. Percutaneous cholecystostomy: a bridge to surgery or definite management of acute cholecystitis in high-risk patients Acute gallstone cholecystitis in the elderly: treatment treatment with emergency ultrasonographic percutaneous cholecystostomy and interval laparoscopic cholecystectomy. Percutaneous cholecystostomy in patients with acute cholecystitis: experience expe- 143. Gallstone recurrence after successful percutaneous cholecystolithotomy: a 10-year follow-up of 439 cases. Percutaneous transhepatic cholecystostomy and delayed laparoscopic cholecystectomy in critically ill patients with acute calculus cholecystitis. Role of percutaneous cholecystostomy for acute acalculous cholecystitis: clinical outcomes of 271 patients. Endoscopic ultrasound-guided rendezvous technique for failed biliary cannulation in benign and resectable malignant biliary disorders. Acute cholecystitis in highrisk patients: percutaneous percutaneous cholecystostomy vs. Equip yourself with trusted, current content that provides you with the clinical knowledge to improve patient outcomes. Kirsner Professor of Medicine Chief, Section of Gastroenterology, Hepatology, and Nutrition Department of Medicine University of Chicago Chicago, Illinois C. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Notice Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. To the fullest extent of the law, no responsibility is assumed by Elsevier, authors, editors or contributors for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products, instructions, or ideas contained in the material herein. Previous editions copyrighted 2016, 2010, 2006, 2002, 1998, 1993, 1989, 1983, 1978, and 1973. Brookes, PhD Associate Professor Australian National University Senior Staff Hepatologist the Canberra Hospital Australian Capital Territory, Australia Daniel C. Cotton Professor of Medicine and Endoscopic Innovation Division of Gastroenterology and Hepatology Medical University of South Carolina, Charleston Charleston, South Carolina, United States Charles O. Hirschowitz Chair in Gastroenterology University of Alabama at Birmingham Birmingham, Alabama, United States Grace H.
Atacand 8mg overnight delivery. Tib A Nabwi s a w w Sy Aids ka Yaqini Elaj Urdu HindiHiv Aids Ka yaqini Elaj urdu By Hakeem Hazik.
Coronal magnetic resonance imaging in T1-weighted image showing circumscribed superior orbital mass hiv infection rate dc buy atacand online pills. Sagittal magnetic resonance imaging in T1-weighted image showing ovoid shape of the superior orbital mass antiviral drug for herpes purchase atacand paypal. Histopathology showing an area of Antoni A pattern with fascicles of nuclei with a ribbon arrangement antiviral research abbreviation generic atacand 8 mg on-line. Once the tumor is removed anti viral oil order atacand with mastercard, the optic disc swelling can resolve and the visual acuity can return to normal hiv infection and aids pictures buy discount atacand 8 mg line. Fundus photograph showing edema of left optic nerve hiv infection window order discount atacand on line, tortuous retinal blood vessels, and choroidal folds. Gross appearance of the circumscribed tumor immediately after removal through a superolateral orbitotomy. Fundus photograph taken 6 months later showing disappearance of the optic disc edema and reversal of the retinal vascular tortuosity. Fluorescein angiogram in the arterial phase 6 months after surgery showing transmission hyperfluorescence corresponding to the persistent choroidal folds. Illustrated is a clinicopathologic correlation of a large schwannoma in a 33-year-old man who declined a recommended neurosurgical approach and sought another opinion to see if it could be removed without a craniotomy. It was removed intact by way of a superolateral orbitotomy despite the fact that it protruded posteriorly through the superior orbital fissure. Appearance of mass immediately after removal by superotemporal orbitotomy with extraperiosteal approach and osteotomy. The nodular protrusion corresponds to where the tumor protruded posteriorly through the superior orbital fissure. Electron photomicrograph of tumor showing wide-spacing collagen in the cytoplasm (Luse body). She had an orbital mass that was found histopathologically after surgical excision to be a schwannoma. On lifting the eyelid, it was found that the left eye had complete absence of ocular motility ("frozen globe"). Magnetic resonance imaging in T1-weighted image, showing elongated mass extending through the optic foramen. Axial magnetic resonance imaging in T2-weighted image, further delineating the well-circumscribed mass. Coronal magnetic resonance imaging showing the location of the mass in the region of the optic foramen. The lesion was removed by a neurosurgical approach and there was no recurrence after 4 years of follow-up. The localized type is clinically and radiographically similar to schwannoma and is associated with neurofibromatosis type 1 in about 10% of cases (25). The diffuse type has a variable association with neurofibromatosis and the plexiform type is almost always seen in association with neurofibromatosis. The histopathologic findings of neurofibroma are discussed in more detail elsewhere (5). Management A patient with suspected localized orbital neurofibroma should be evaluated and managed as described for other localized orbital tumors. Clinical findings and imaging studies should be done and complete surgical excision should be considered for symptomatic lesions. However, surgical intervention is often necessary because of bothersome symptoms, threatened vision, or an unacceptable cosmetic appearance. In such instances, debulking surgery is often done, because complete surgical removal may not be possible. Depending on the extent of the disease, a combined approach with neurosurgeons and otolaryngologists may be prudent (19,24). Clinical Features Localized neurofibroma produces clinical symptoms and signs similar to schwannoma and other circumscribed orbital tumors and can manifest as proptosis, globe displacement, diplopia, and optic nerve compression. It is usually diagnosed in middle-aged or adult patients and, as mentioned, does not occur in patients with neurofibromatosis type 1. Localized neurofibroma can sometimes occur as multiple orbital tumors in patients without clear evidence of neurofibromatosis. Diffuse and plexiform neurofibromas are very similar clinically and radiographically, but are classified separately because of subtle histopathologic differences (5). They generally become clinically apparent in the first decade of life and show gradual progression, often with involvement of other periocular and ocular tissues, including the uveal tract. The diffuse, poorly defined mass can cause the classic S-shaped curve to the upper eyelid owing to subcutaneous involvement by the tumor. The plexiform form can be very extensive with massive involvement of the orbit, eyelids, and intraocular structures. In addition, patients with neurofibromatosis can have congenital defects in the sphenoid bone that can produce a characteristic pulsating proptosis similar to that seen with encephalocele. Diagnostic Approaches With orbital computed tomography and magnetic resonance imaging, localized neurofibroma appears as a circumscribed mass that is indistinguishable from schwannoma, described previously (6). Plexiform and diffuse neurofibromas show an irregular, ill-defined mass, often with extensive periorbital involvement, as mentioned. Pathology Localized orbital neurofibroma is circumscribed but lacks a true capsule. The classical case shows interlacing bundles of elongated spindle cells with variable quantities of mucoid material. Diffuse and plexiform neurofibromas are composed of a complex intertwining of bundles of enlarged nerves with proliferation of Schwann cells and endoneural fibroblasts in a mucoid Chapter 29 Orbital Peripheral Nerve Tumors 563 Selected References 1. Use of the carbon dioxide laser in the management of orbital plexiform neurofibromas. Another orbital manifestation is pulsating proptosis secondary to absence of the greater wing of the sphenoid bone but without an obvious tumor. Blepharoptosis and proptosis of the right eye in a 6-yearold boy with plexiform neurofibroma of the orbit. Note the advanced diffuse orbital tumor and the long section of grossly normal optic nerve. Note the absence of the sphenoid bone that allowed brain pulsations to be transmitted to the orbit. Chapter 29 Orbital Peripheral Nerve Tumors 565 Orbital Neurofibroma: Progression of Eyelid, Orbital, and Intraocular Neurofibromatosis In some instances, neurofibromatosis can involve almost every ocular structure and can demonstrate progressive growth and attain large proportions. One-month-old girl with type 1 neurofibromatosis involving the eyelid, orbit, and globe. Same child at age 4 months showing progression of proptosis and development of a cataract. Same child at 18 months showing progression of eyelid mass, proptosis, and subcutaneous involvement of right side of face. After much counseling, the parents requested attempted tumor debulking of the tumor and enucleation of the blind right eye, partly for cosmetic reasons. There is surgical anophthalmos but massive subcutaneous and orbital involvement continues to progress. Pathology of plexiform neurofibroma of orbit from same child showing enlarged nerve bundles typical of plexiform neurofibroma. A clinicopathologic correlation with computed tomography and magnetic resonance imaging in a 35-year-old woman is illustrated. Coronal computed tomography showing superior orbital mass with cystlike central portion. Coronal magnetic resonance imaging in T1-weighted image showing the superior orbital mass with low signal component. In the 58-year-old man illustrated here, there was no clinical evidence of neurofibromatosis except for three separate neurofibromas in the right orbit. It is possible that it could represent a forme fruste of von Recklinghausen neurofibromatosis. Proptosis of the right eye, which had been slowly progressive and painful for several years. Axial computed tomography showing retrobulbar mass and a separate mass in the temporal fossa. Coronal computed tomography showing the retrobulbar mass and a third mass in the inferior aspect of the orbit with displacement of the bony floor of the orbit. Appearance of the retrobulbar mass immediately after surgical removal of all three tumors. Multiple locations are involved in 10% to 20% of cases, especially if there is a familial predisposition (2). Prognosis the visual and systemic prognosis is generally good for patients with orbital paraganglioma. Paraganglioma of the orbit with extension to the middle cranial fossa: case report. Clinical Features Orbital paraganglioma can become apparent at any age with reported cases having their onset between 4 and 55 years (7). It has been reported to extend from the orbit into the middle cranial fossa (10) and to secondarily invade the orbit from an intracranial primary location (5). Diagnostic Approaches With imaging studies, orbital paraganglioma is usually a wellcircumscribed tumor that enhances with contrast agents and is often attached to a rectus muscle. Pathology and Pathogenesis Paraganglioma is an encapsulated tumor composed of clusters and nests of cells, called "zellballen" that are separated from one another by delicate vascularized septae, and that give the tumor a distinctive pseudoalveolar arrangement. Ultrastructurally, paraganglioma has small, dense core granules measuring 1,000 to 2,000 angstroms in diameter. The pathogenesis of paraganglioma is unknown, but some cases are familial and multifocal, suggesting a genetic mutation that is still undetermined. Management Orbital paraganglioma is almost never diagnosed clinically because it is rare and has no specific features. Axial magnetic resonance imaging in T1-weighted image in a 53-year-old man who presented with proptosis of left eye showing gadolinium enhancement of circumscribed, elongated mass filling most of the orbit. Among the 17 patients, the mean age at diagnosis was 23 years and median age 18 years, with a range of 11 months to 69 years. If not treated early and effectively, it can become alarmingly aggressive and can fill the orbit and destroy the globe. The loosely cohesive cells sometimes float freely in the alveolar spaces, resembling the alveolar variant of rhabdomyosarcoma. A characteristic feature is the presence of typical periodic acidSchiff-positive, diastase-resistant intracytoplasmic crystalline structures that can be better demonstrated with electron microscopy (5,6,8). A leading possibility is that it represents a tumor of neural origin, perhaps a malignant variant of a paraganglioma (chemodectoma) or granula cell tumor (1,2). Alveolar soft-part sarcoma of the orbit: a clinicopathologic analysis of seventeen cases and a review of the literature. The ultrasonographic and radiologic features of a histologically proven case of alveolar soft-part sarcoma of the orbit. Histopathology of orbital alveolar soft-part sarcoma demonstrating the alveolar arrangement of the cells and periodic acidSchiff-positive crystals in cytoplasm. The child was treated elsewhere with corticosteroids with a diagnosis of orbital inflammatory pseudotumor, but the lesion continued to progress and biopsy revealed alveolar soft part sarcoma. Appearance of the patient 3 months later showing marked progression of the lesion. Histopathology showing periodic acid-Schiff-positive, diastase-resistant intracytoplasmic structures in the tumor cells. In the ocular region, it has been known to appear in the conjunctiva, caruncle, lacrimal sac, eyebrows, eyelids, and, rarely, the iris (11). Approximately 10% to 15% of reported cases from extraocular areas have been multifocal (2), but the orbital cases have all been solitary. This concept was supported by the fact that the tumor frequently occurred in the oral cavity, particularly the tongue. Like other slowly progressive, circumscribed, benign tumors, the best management is complete surgical excision if possible. Granular cell tumor of the orbit: A case report including electron microscopic observation. Granular cell tumor of the eye (myoblastoma): ultrastructural and immunohistochemical studies. The clinical features are nonspecific and most cases are not suspected clinically, but are diagnosed histopathologically after surgical excision. The close relationship to muscle in some cases does not negate the possibility of a neural origin, because it can arise from a nerve in proximity to the muscle. Special stains and immunohistochemistry can assist in the differential diagnosis (2). The cytoplasm is intensely periodic acid-Schiff positive and diastase resistant, suggesting that the granules are not glycogen and thereby excluding the likelihood of a muscle tumor. They are desmin positive and S-100 protein positive, supporting a neural crest origin. Ultrastructural studies show abundant intercellular basement membrane and spindle cells that may contain characteristic cytoplasmic inclusions called angulated or Bangle bodies (2). Chapter 29 Orbital Peripheral Nerve Tumors 575 Orbital Amputation Neuroma General Considerations Amputation neuroma occurs at the stump of severed peripheral nerves and can produce "phantom limb" symptoms. There were no cases in the Wills Eye Hospital clinical series (8) or in the Mayo Clinic series (1).
Sardian Nut (European Chestnut). Atacand.
- Are there safety concerns?
- Bronchitis, whooping cough, nausea, diarrhea, stomach problems, circulation problems, fever, infections, kidney disorders, muscle pain, sore throat, wounds, and other conditions.
- Dosing considerations for European Chestnut.
- Are there any interactions with medications?
- What is European Chestnut?
- How does European Chestnut work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96522


















