Minomycin

Peter C. Gerszten, MD, MPH, FACS
- Associate Professor
- Department of Neurological Surgery and Radiation Oncology
- University of Pittsburgh Medical Center
- Pittsburgh, Pennsylvania
Because sensory and motor functions are anatomically relatively distant in the cerebral cortex but progressively closer together as fibers converge in the brain stem treatment for dogs going blind purchase cheap minomycin line, spinal cord antibiotics quinsy buy minomycin in united states online, roots antimicrobial quizzes purchase minomycin 100 mg without a prescription, and peripheral nerves virus vector cheap generic minomycin uk, the coexistence of sensory loss and motor dysfunction in a limb implies a large lesion at the level of the cortex or a smaller lesion lower down in the neuraxis tetracycline antibiotics for acne treatment order genuine minomycin on-line. Small lesions in areas of high traffic such as the spinal cord or brain stem can result in widespread neurologic dysfunction antibiotic blue pill discount generic minomycin canada, whereas small lesions elsewhere may be asymptomatic. Some symptoms can result from a lesion at any of several levels of the nervous system. Associated symptoms (or their lack) may lead the interviewer to reject certain hypotheses that at first seemed most likely. Some neuroanatomic locations point to a specific diagnosis or a limited number of diagnoses. For example, disease of the neuromuscular junction is usually caused by an autoimmune process such as myasthenia gravis (common) or Eaton-Lambert myasthenic syndrome (uncommon). Certain symptoms such as double vision almost invariably develop abruptly, even if the underlying disorder has been developing gradually over days to weeks. Unexpected signs must be explained, often with a return to the history for further clarification. The goal of the exam is to determine whether the cause is diffuse, focal or multifocal. In the case of the motor system, the final common pathway is the motor unit and includes the anterior horn cells giving rise to axons in a nerve, the nerve itself, the neuromuscular junction, and the muscle. Conversely, if these structures are intact, observing the muscle function may be possible under the right circumstances. If all modes of engaging the final common pathway fail to elicit a response, the clinician can conclude that the lesion is located somewhere within the final common pathway. Tissue infection in the region of the puncture site is an absolute contraindication to lumbar puncture. Relative contraindications include known or probable intracranial or spinal mass lesion, increased intracranial pressure as a result of mass lesions, coagulopathy caused by thrombocytopenia (usually correctable), anticoagulant therapy, and bleeding disorders. Rare but severe complications of lumbar puncture include transtentorial or foramen magnum herniation, spinal epidural hematoma, spinal abscess, herniated or infected disk, meningitis, and adverse reaction to a local anesthetic agent. If the problem is central, however, facial movement with involuntary (spontaneous) smiling may be preserved or increased. Central input to a final common pathway in the nervous system is usually tonically inhibitory. Damage to this input typically results in overactivity of the involved muscle group. Signs of damage to central inhibitory systems include spasticity and hyperreflexia. Testing should be selectively performed because of expense, risk, and discomfort to the patient. Diagnostic tests should never be ordered without a specific differential diagnosis firmly in mind. Additional, special studies may be obtained as appropriate, including Gram stain; fungal, viral, and tuberculous cultures; cryptococcal and other antigens; tests for syphilis; Lyme titers; malignant cytologic patterns; paraneoplastic and other specific protein antibodies; and oligoclonal bands. The 14-3-3 protein, found in Creutzfeldt-Jakob disease, may be found in patients with rapid-onset dementia. Occasionally, biopsy provides the only means of arriving at a definitive diagnosis. Electrophysiologic Studies Electrophysiologic studies include electroencephalography, electromyography, nerve conduction studies, and evoked potentials. These studies are helpful in situations in which the patient cannot be examined or interviewed adequately. Electroencephalography is most often used to investigate seizures (see Chapter 120). It can document encephalopathy, in which case the background electrical activity of the brain is slowed, and it is also used in the evaluation of brain death. Electromyography is useful in the differential diagnosis of muscle disease, neuromuscular junction disease, peripheral nerve disease, and anterior horn cell disease. Nerve conduction studies (see Chapters 123 and 124) may show decreased amplitude (characteristic of axonal neuropathy) or decreased velocity (characteristic of demyelinating neuropathy). Visual-evoked potential studies are commonly used in the evaluation of possible multiple sclerosis (see Chapter 122). Asymmetrical slowing of the cortical response to visual pattern stimulation suggests demyelination in the optic nerve or central optic pathways. Lesions at the cerebellopontine angle and the brain stem cause abnormal delay in conduction. Brain stem auditory-evoked potentials are helpful in the diagnosis of deafness in infants. Somatosensory-evoked potentials are used to identify a slowing of central sensory conduction that results from demyelinating disease, compression, or metabolic derangements. For example, upper motor neurons converge on lower motor neurons, whose axons form the final common pathway to an effector muscle. Genetic and Molecular Testing There are more neurologic diseases than diseases of all other systems combined. Discoveries have revolutionized the diagnostic approach to many of these diseases, and new genetic tests are discovered every year. Important ethical issues surround the use of genetic tests, including the ability to ensure privacy, to ensure adequate psychological and social support for patients who may be given devastating news, and to address adequately the appropriateness of prenatal screening or presymptomatic testing when no treatment is available. Studies of previously untreatable neurodegenerative disorders are now targeting presymptomatic individuals in the hope that earlier intervention can modify disease outcomes. Despite these and foreseeable future advances, the clinical aspects of neurologic disease remain fundamentally important in understanding the impact of disease on patients and their families. Noninvasive ultrasonography of the carotid and vertebral arteries can define stenotic vessels. It has been supplemented by transcranial Doppler technology, which allows characterization of blood flow in intracranial arteries. Biller J, editor: Practical neurology, ed 4, Philadelphia, 2012, Lippincott Williams & Wilkins. A poorly responsive state in which the eyes are spontaneously open, or an agitated and confused state, or delirium is not coma but may represent early stages of the same disease processes and should be investigated in the same manner. Consciousness requires that the brain stem reticular activating system and its cortical projections be intact and functioning. The reticular formation begins in the mid pons and ascends through the dorsal midbrain to synapse in the thalamus; it then innervates higher centers through thalamocortical connections. In addition to structural lesions, meningeal inflammation, metabolic encephalopathy, sedation, and seizures diffusely affect the brain and complete the differential diagnosis for the patient in coma. Metabolic abnormalities result in diffuse dysfunction of the nervous system; therefore, with rare exceptions, they produce no localized signs such as hemiparesis or unilateral papillary dilation. The diagnosis of metabolic encephalopathy means that the examiner has found no focal anatomic features on examination or neuroimaging studies to explain coma but that a specific metabolic cause has not been established. Drugs have a predilection for affecting the reticular formation in the brain stem and for producing paralysis of reflex eye movement on examination. In the late stages of status epilepticus, motor movements may be subtle even though seizure activity is continuing throughout the brain (nonconvulsive status epilepticus). Once seizures stop, the so-called postictal state can also cause unexplained coma. A history of a premonitory headache supports a diagnosis of meningitis, encephalitis, or intracerebral or subarachnoid hemorrhage. A preceding period of intoxication, confusion, or delirium points to a diffuse process such as meningitis or endogenous or exogenous toxins. The sudden apoplectic onset of coma is particularly suggestive of ischemic or hemorrhagic stroke affecting the brain stem or of subarachnoid hemorrhage or intracerebral hemorrhage with intraventricular rupture. Lateralized symptoms of hemiparesis or aphasia before coma occur in patients with hemispheric masses or infarctions. Hemispheric mass lesions result in coma either by expanding across the midline laterally to compromise both cerebral hemispheres or by impinging on the brain stem to compress the rostral reticular formation. These processes-lateral herniation (lateral movement of the brain) and transtentorial herniation (vertical movement of the brain)- most commonly occur together. Brain stem mass lesions produce coma by directly affecting the reticular formation. Because the pathways for lateral eye movements-the pontine gaze center, medial longitudinal fasciculus, and oculomotor (third nerve) nucleus-traverse the reticular activating system, impairment of reflex eye movements is often the critical element of diagnosis of a brain stem lesion. A comatose patient without impaired reflex lateral eye movements does not have a mass lesion compromising brain stem structures in the posterior fossa. Posterior fossa lesions may block the flow of cerebrospinal fluid from the lateral ventricles, resulting in the dangerous situation of noncommunicating hydrocephalus. Identification of Meningitis Signs of meningeal irritation are not invariably present and have differing sensitivities depending on the cause: They are extremely common with acute pyogenic meningitis and subarachnoid hemorrhage and less common with indolent, fungal meningitis. Nevertheless, the presence of these signs on examination is the central clue to the diagnosis. Missing these signs results in time-consuming additional tests such as brain imaging and the potential loss of a narrow window of opportunity for directed therapy. The terms early diencephalic and late diencephalic refer to levels of dysfunction just above and just below the thalamus, respectively. Because the evaluation and potential treatments for structural and metabolic coma are widely divergent and the disease processes in both categories are often rapidly progressive, initiating prompt medical and surgical evaluation may be life-saving. Identification of a structural versus a metabolic cause is accomplished by focusing on three features of the neurologic examination: the motor response to a painful stimulus, pupillary function, and reflex eye movements. When the neck is passively flexed by attempting to bring the chin within a few fingerbreadths of the chest, patients with irritated meninges reflexively flex one or both knees. This sign, called the Brudzinski reflex, is usually asymmetrical and not dramatic, but any evidence of knee flexion during passive neck flexion mandates that the cerebrospinal fluid be examined. Although rare cases of herniation after lumbar puncture have been reported in children with bacterial meningitis, the urgency of diagnosis and treatment at the point of coma is paramount. An alternative approach involves obtaining blood cultures and immediately initiating antibiotic therapy with subsequent lumbar puncture. With this approach, the cerebrospinal fluid cell count, glucose determination, and protein content are unchanged, and Gram stain and culture often remain positive despite a short period of antibiotic treatment. Asymmetrical or reflex function of the motor system provides the clearest indication of a mass lesion. Elicitation of a motor response requires that a painful stimulus be applied, to which the patient will react. Strong pressure on the supraorbital ridge or pinching of the skin on the anterior chest or inner arm is the most useful method; finger nail bed pressure is also used, but it makes the interpretation of upper limb movement difficult. This lateralized motor response in a comatose patient establishes the working diagnosis of a hemispheric mass. As the mass expands to involve the thalamus (late diencephalic stage), the response to pain becomes reflex arm flexion associated with extension and internal rotation of the legs (decorticate posturing); asymmetry of the response in the upper extremities is seen. It has a rapid onset and rapid recovery, often with myoclonic jerking and confusion. It causes deep coma lasting 2 to 3 hours (Glasgow Coma Scale score = 3) with maintenance of vital signs. Obtain blood for glucose, electrolytes, hepatic and renal function, prothrombin and partial thromboplastin times, complete blood count, and drug screen. A small amount of asymmetrical flexion or extension of the arms in response to a painful stimulus carries the same implications as the full-blown postures of decortication or decerebration. Metabolic lesions do not compromise the brain in a progressive, level-by-level manner as do hemispheric masses, and they rarely produce the asymmetrical motor signs typical of masses. Reflex posturing may be seen, but it lacks the asymmetry of decortication seen with a hemispheric mass, and it is not associated with the loss of pupillary reactivity at the stage of decerebration. Pupillary Reactivity In metabolic coma, one feature is central to the examination: Pupillary reactivity is present. This reactivity is seen both early in metabolic coma, when an appropriate motor response to pain may be retained, and late in coma, when no motor responses can be elicited. The pupillary reaction in metabolic coma is lost only when coma is so deep that the patient requires ventilatory and blood pressure support. At this point, the pupils become mid-position in size, and the light reflex is lost, first unilaterally and then bilaterally. With further progression to the level of the pons, the most frequent finding is no response to painful stimulation, although spinal-mediated movements of leg flexion may occur. Reflex lateral eye movements, the pathways for which traverse the pons and midbrain, are particularly affected, and the reflex postures of decortication and decerebration typical of brain stem injury are common. Ocular bobbing (spontaneous symmetrical or asymmetrical rhythmic vertical ocular oscillations) is most often a manifestation of a pontine lesion. Seizures occurring in a patient with acute brain injury (such as that resulting from encephalitis, hypertensive encephalopathy, hyponatremia, hypernatremia, hypoglycemia, or hyperglycemia) or chronic brain injury (such as dementia or mental retardation) often result in prolonged postictal coma. The examination shows reactive pupils and inducible eye movements (in the absence of overtreatment with anticonvulsants), and often up-going toes or focal signs are observed (Todd paresis). Nonconvulsive status epilepticus should be considered as a diagnosis even if there are no obvious seizure movements. Nonconvulsive seizures can cause coma and also can complicate other etiologies of coma, including infectious and metabolic disorders. Nonconvulsive seizures should be suspected in patients with (1) a seemingly prolonged "postictal state" after generalized convulsive seizures or prolonged alteration of alertness after an operative procedure or neurologic insult; (2) acute onset of impaired consciousness or fluctuating mentation interspersed with episodes of normal awareness; (3) altered mental status or consciousness associated with facial myoclonus or nystagmoid eye movements; or (4) episodic blank staring, aphasia, automatisms. Current evidence suggests that the presence of nonconvulsive seizures or periodic discharges, delay to diagnosis, and duration of nonconvulsive status in patients with or without acute brain injury are independent predictors of worse outcome. Pupillary, corneal, and motor responses are the best clinical indicators of prognosis that can be assessed at bedside. Although the neurologic exam is still the cornerstone of prognostication, there has been extensive work using other modalities to better predict prognosis.
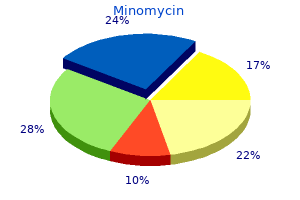
Major depression is common infection x ray purchase minomycin 50 mg overnight delivery, with a 12-month prevalence of approximately 7% and a lifetime prevalence of up to 10% among men and 20% to 25% in women antibiotics yeast infection treatment buy minomycin 50mg cheap. First onset may occur at any age but is most common in the third through fifth decades of life virus protection for windows xp purchase minomycin 100 mg free shipping. Whereas most episodes of major depression fully remit spontaneously or with treatment can i get antibiotics for acne order 100 mg minomycin visa, the lifetime risk of recurrence is at least 50% to 70% antimicrobial effectiveness testing cheap 50 mg minomycin with mastercard, and up to 20% of patients may experience chronic symptoms over many years antibiotics for uti otc order line minomycin. Major depression is a leading correlate of disability worldwide, is an important determinant of death by suicide, and is associated with increased risk of death from comorbid physical illnesses. Major depression also causes significant economic burden, costing approximately 210. Depressive disorders are heterogeneous, with many potential pathogenic mechanisms. Genetic factors, such as polymorphisms of the serotonin transporter protein, affect vulnerability to depressive episodes in the face of psychosocial stressors. Depression is polygenic and multifactorial, with genetic factors accounting for about 40% of the risk. Alterations in the functioning of brain serotonergic and noradrenergic systems and of the hypothalamic-pituitary-adrenal axis are found in depression. Neuroimaging studies show smaller hippocampal volumes and altered metabolic activity in several regions, including the anterior cingulate cortex. However, the information in these studies is not sufficient for making the clinical diagnosis, which depends on identification of the clinical syndrome. Dysfunctional, negativistic patterns of thinking, impaired social relationships, and stressful life events also contribute to depression. Mild to moderate forms of major depression respond to focused psychotherapies or antidepressant medications (Table 111. More severe forms of depression do not respond to psychosocial interventions alone. Severe or refractory depression may be treated safely and effectively with electroconvulsive therapy. Other evidence-based somatic therapies include light therapy (for depression with a seasonal component) and vagal nerve stimulation. Manic episodes include elevated (euphoric) or irritable mood, goal-directed hyperactivity (often for pleasurable activities with poor judgment leading to substantial adverse consequences such as sexual, spending, or gambling sprees), pressured speech, increased energy level with a decreased need for sleep, and distractibility. Compared with unipolar depression, bipolar disorder has a lower 12-month prevalence (approximately 0. Most patients return to baseline functioning between acute mood episodes, but some have a deteriorating course, and others have frequent debilitating episodes. Genetic factors play a greater role in the pathogenesis of bipolar disorder than in major depressive disorder, accounting for approximately 50% of the risk and representing a greater than 50-fold increase over the population base rate. Bipolar disorder is polygenic and has been linked in individual families to different loci. The pathogenesis is unclear but likely involves dysregulation of frontostriatal systems. Structural neuroimaging studies show increased ventricular-to-brain ratios, suggesting parenchymal atrophy. Psychosocial stressors often play a role in precipitating episodes of mania and depression. Antipsychotic medications are useful for acute manic episodes and may have a role in maintenance therapy. Benzodiazepines may be used to treat acute agitation and aggression while waiting for more definitive antimanic therapies to take effect. Antidepressants have long been used for depressive episodes, although they may precipitate manic episodes. Psychosocial treatments alone do not effectively treat mania and may be less effective for bipolar depression, but psychoeducation and support to manage psychosocial stressors and encourage medication compliance improve longer-term outcomes. A spectrum of less severe bipolar disorders includes conditions marked by episodes of hypomania. A panic attack is a transient episode of crescendo anxiety, catastrophic thoughts. If panic attacks or other clinically significant anxiety symptoms occur only in predictable response to environmental stimuli, the anxiety disorder is known as a phobia, which may further be classified as agoraphobia. Panic disorder manifests with recurrent panic attacks, some of which are unexpected and unpredictable, along with anticipatory anxiety. Enduring anxiety in various domains that the individual finds difficult to control is classified as generalized anxiety disorder. Those with generalized anxiety disorder may also experience physical symptoms such as feeling keyed up, muscle tension or fatigue; however, they are not in discrete episodes. Recognizing its distinct pathogenesis involving striatofrontal function and central serotonergic systems, it has been classified separately from the anxiety disorders. Individuals exposed to severely stressful events (typically involving the actual or threatened loss of life or limb) may experience any of a wide variety of psychiatric sequelae. These disorders also have been classified separately, as in addition to anxiety symptoms, they can present with prominent dysphoric symptoms, externalizing aggressive symptoms, or dissociative symptoms. These disorders are common, with point prevalence of 1% to 2% each for panic disorder and obsessive-compulsive disorder and up to 10% for phobias. Although there are fewer data on long-term outcome than for mood disorders, many of these disorders tend to have a chronic waxing and waning course. Although new-onset anxiety is common in later life, the cause is rarely a late-onset primary anxiety disorder (see Table 111. The pathogeneses of most anxiety disorders may be understood as inappropriate activation of the stress response system involving a variety of neuroendocrine and autonomic outputs and coordinated by the central nucleus of the amygdala and other brain structures. The amygdala receives excitatory glutamatergic inputs from cortical sensory areas and the thalamus and has outputs to the major monoaminergic centers. They are the sole therapies for specific phobias and may be the sole or primary therapy for most other anxiety disorders or combined with pharmacotherapy. Increasingly, antidepressant medications have replaced anxiolytics as the mainstay of pharmacotherapy for panic disorder, post-traumatic stress disorder, generalized social phobia, and generalized anxiety disorder. For obsessive-compulsive disorder, only antidepressant agents with pronounced activity on the serotonergic system. Schizophrenia is the prototypic psychotic disorder; it includes acute episodes of psychosis. Peak onset is in late adolescence to young adulthood, with slightly younger ages for males than females. The annual incidence is approximately 15 cases per 100,000 people, but with marked variability across study samples and populations. The pathogenesis of schizophrenia remains unknown, but it is clearly multifactorial. Studies of postmortem brains indicate a nongliotic neuropathologic process with subtle disruptions of cortical cytoarchitecture. It is likely that psychosocial factors and neurodevelopment interact with a nonlocalizable brain lesion present at birth or acquired early in life. Dopaminergic mesocortical and mesolimbic pathways are important in the production of psychotic symptoms. Antipsychotic medications, often with adjunctive benzodiazepines, are used to treat acute psychotic episodes (Table 111. Although maintenance antipsychotic medications help reduce the severity and frequency of acute psychotic episodes, comprehensive psychosocial rehabilitation programs are required to help patients manage interpersonal and other stressors and to improve overall clinical outcomes. Adjunctive cognitive-behavioral therapy also may improve outcomes for some patients. However, second-generation drugs contribute to an increase in obesity and metabolic syndrome. Schizoaffective disorder is a chronic, recurrent disorder with a prevalence slightly lower than that of schizophrenia. The outcomes of schizoaffective disorder are heterogeneous but on average are intermediate between schizophrenia and mood disorders. Treatment is symptomatic, using antipsychotic, mood stabilizing, and antidepressant medications to target specific psychotic and mood symptoms. Delusional disorder is characterized by delusions in the absence of thought process disorder, prominent hallucinations, or the negative symptoms of schizophrenia. The pathogeneses of the non-schizophrenic primary psychotic disorders remain largely unknown. In the future, precision medicine in psychiatry will allow us to use information such as genomics and brain imaging to more accurately define, diagnose, and treat illness. The recent approval of two drugs with different mechanisms of action from previous antidepressants, intranasal esketamine and brexanolone, exemplifies the potential to discover new ways to treat mood and other psychiatric disorders. What is particularly exciting regarding these new medications is that they appear to work more quickly than other antidepressants. It remains to be seen how they will be optimally deployed among other therapeutic choices. Prevention remains an important area of growth in psychiatry, albeit an area that historically had lagged behind many other medical specialties. Promising data showing that early intervention teams for patients suffering from first onset psychosis improve long-term outcomes is a step in the right direction. Evidence is also growing that late-life depression can be prevented by cost-effective preventive interventions in at-risk patients in primary care and several specialty settings. Advances in prevention, diagnosis, and treatment will contribute to a new understanding of mental illness and lead to a future in which the global burden of mental illness can be decreased. Malingering is the conscious feigning of illness for conscious gain and therefore is not a mental disorder. For example, a patient who exhibits dependent features solely while acutely depressed does not have a dependent personality. A personality disorder is diagnosed when personality traits lead to pervasive (if variable) subjective distress or dysfunction in a broad range of situations. Personality and personality disorders are the result of complex interactions among genetic, environmental, and developmental factors. Approaches to patients with personality disorders depend on the specific type, but in most clinical circumstances other than long-term psychotherapy, the realistic goal is not to alter fundamental personality structure but to help the patient maximize use of personality strengths. Although not the mainstay of most treatments for personality disorders, pharmacotherapy can be useful in selected patients. Patients with personality disorders are also prone to mood, anxiety, eating, addictive, and other treatable psychiatric disorders. Its central network and peripheral sympathetic and parasympathetic divisions integrate complex organ functions, maintain internal homeostasis in response to environmental change, modulate the flight-or-fight physiologic response to stress, and enable circulation, digestion, and procreation. Neurally mediated syncope and situational reflex syncope in response to emotional distress, carotid sinus stimulation, micturition, defecation, coughing, straining, or other factors occur in about 20% of people during a lifetime and account for 1% to 3% of all emergency room visits. One of the most disabling manifestations of autonomic failure is orthostatic hypotension, the prevalence of which increases with age, physical inactivity, and in diseases that impair sympathetic adrenergic nerves. Diabetes mellitus is the most common cause of autonomic neuropathy in industrialized nations. About 30% of diabetics develop autonomic neuropathy, and symptomatic orthostatic hypotension occurs in 5% of patients. Other features of autonomic neuropathy include constipation in 40% to 60% of diabetics, gastroparesis in 20% to 40%, bladder dysfunction in 30% to 80%, and erectile impotence in more than 30% of men. For a deeper discussion of these topics, please see Chapter 22, "Common Clinical Sequelae of Aging," and Chapter 216, "Diabetes Mellitus," in Goldman-Cecil Medicine, 26th Edition. They include a wide range of degenerative, traumatic, cerebrovascular, autoimmune, genetic, metabolic, toxic, and pharmacologic conditions. Small-caliber peripheral autonomic nerves are unmyelinated or thinly myelinated, and small-fiber peripheral neuropathies that cause distal sensory loss may also involve sympathetic or parasympathetic nerves. Diabetic autonomic neuropathy results from microvascular damage to autonomic nerves. Several hereditary, infectious, metabolic, toxic, and drug-induced sensory and autonomic neuropathies are recognized causes. Accumulation of abnormal proteins distinguishes some of the degenerative dysautonomias. Oligodendroglial cytoplasmic inclusions composed of aggregates of misfolded -synuclein are pathognomonic of multiple system atrophy. The list of autoimmune autonomic neuropathies includes acute autonomic ganglionopathy; patients with acute pandysautonomia have antibodies against the nicotinic acetylcholine receptor in autonomic ganglia, which is sometimes associated with lung cancer or thymoma. Additional paraneoplastic autonomic neuropathies include those associated with antineuronal nuclear antibody type 1. Lambert-Eaton myasthenic syndrome is associated with antibodies to voltage-gated calcium channels. Antibodies to voltage-gated potassium channels cause autoimmune neuromyotonia and dysautonomia with hyperhidrosis and orthostatic intolerance. Diuretics, sympatholytic drugs, -adrenoreceptor blockers, and vasodilators can cause or contribute to orthostatic hypotension. Anticholinergics and carbonic anhydrase inhibitors decrease sweating, whereas opioids and selective serotonin reuptake inhibitors increase sweating. Anticholinergics, tricyclic antidepressants, and antihistamines may cause urinary retention.
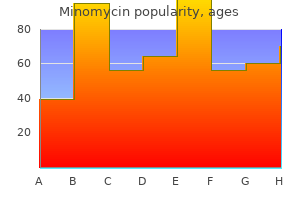
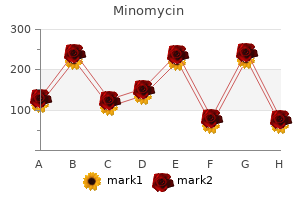
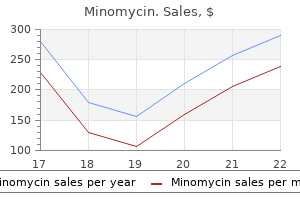
Lymphoid Leukemias Acute Lymphocytic Leukemias the acute lymphocytic leukemias that arise from precursor B or T cells are described in detail in Chapter 47 virus game app minomycin 100mg low cost. Chronic Lymphocytic Leukemia and Small Lymphocytic Lymphoma Definition and epidemiology antimicrobial 10 minomycin 100mg otc. Although it can occur at any stage of life virus living or non living purchase minomycin online from canada, the incidence increases with age infection and immunity cheap minomycin 50 mg line, and more than 90% of cases are diagnosed in adults older than 50 years of age termin 8 antimicrobial preservative minomycin 100mg. The rate of rise of the white blood cell count may also be used to predict development of symptoms and the need for therapy antibiotic 3 days uti purchase cheap minomycin. Patients with del(17p) did not respond to fludarabine-based regimens, however, and had a median survival of only 16 months after first-line treatment. Some of these patients have not relapsed with over 10 years of follow-up and may have been cured. Patients with recurrent or refractory disease may respond to a growing list of monoclonal antibodies. At 3 years of follow-up an unprecedented 50% of del(17p) patients taking ibrutinib were alive without progression of disease. The most frequent abnormalities involve chromosomes 12 (often trisomy 12), 13, and 14. Cytogenetic abnormalities of chromosomes 17 and 11 are associated with an adverse prognosis. Smears of the bone marrow or peripheral blood reveal a predominance of small lymphocytes with inconspicuous nucleoli; ruptured cells. Examination of involved lymph nodes reveals a diffuse infiltrate of small lymphocytes effacing the normal architecture. Some patients exhibit lymphadenopathy, symptoms related to cytopenias, or recurrent infections. As the disease progresses, patients develop generalized lymphadenopathy, hepatosplenomegaly, and bone marrow failure. Patients who develop autoimmune phenomena require treatment with corticosteroids, and intravenous gamma globulin may be used to reduce the frequency of infections in patients who have developed hypogammaglobulinemia. M proteins can be found in benign and malignant conditions other than the plasma cell dyscrasias (Table 50. M proteins can also be detected in a variety of autoreactive or infectious disorders. Multiple myeloma is a malignant plasma cell disorder characterized by neoplastic infiltration of the bone marrow and bone and by monoclonal immunoglobulin or light chains in the serum or urine. The disease is more common in men than women and in African Americans than white individuals. Myeloma risk is increased for patients with first-degree relatives with a plasma cell dyscrasia. Associations have been described with occupational exposures to organic solvents, pesticides, petroleum products, and ionizing radiation; however, most patients with myeloma have no history of exposure to such agents. The tumor cell exhibits features of a differentiated plasma cell that is adapted to synthesize and secrete immunoglobulin at a high rate. Biopsies of bone marrow or targeted bone biopsies of tumor sites reveal infiltration by plasma cells with light-chain restriction, defining clonality. Genetic aberrations are detectable in most patients with myeloma if adequately sensitive tests are applied. The diagnosis of multiple myeloma is made by identifying some combination of an increase (>10%) in the number of plasma cells in the bone marrow, a serum M protein other than IgM exceeding 3 g/dL, or a clonal protein in the urine. Recurrent infection with hypogammaglobulinemia is also considered a criterion for symptomatic myeloma. Evaluation of the patient with suspected myeloma includes bone marrow biopsy; measurement of hemoglobin, calcium, renal function, and the serum free -to- light-chain ratio; serum and urine protein electrophoresis; immunoelectrophoresis; and a skeletal survey. The laboratory hallmark of plasma cell dyscrasias is a homogeneous immunoglobulin molecule (whole or part) that can be detected in the serum or urine by protein electrophoresis. Clinically, these disorders may be characterized by the systemic effects of the M protein and by the direct effects of bone and bone marrow infiltration. Primary amyloidosis, for instance, results in tissue injury through deposition of light chains produced by a clonal population of plasma cells in the absence of an observable proliferation of the plasma cell clone. It is discussed in this section because of the distinct clinical effects of the IgM paraprotein produced in this disease. The risk of progression is greater among patients with IgA or IgM-type M proteins, in patients with initial concentrations of M protein in excess of 1. About 20% of patients with multiple myeloma do not have detectable serum M protein by standard electrophoresis but have circulating free light chains that may be detectable by serum free light-chain assays. Free light-chain assays are quite sensitive and may provide measurement of clonal protein in patients thought to have non-secretory disease by other methods. Free light chains have a relatively short half-life (2 to 6 hours) in the circulation compared with a half-life of weeks for intact immunoglobulin molecules and may therefore be used to obtain a more rapid assessment of disease response once therapy is initiated. In rare cases, patients may have true non-secretory myeloma with no detectable serum or urine M protein by any assay. The clinical manifestations of multiple myeloma are the direct effects of bone marrow and bone infiltration by malignant plasma cells, the systemic effects of the M protein, and the effects of the concomitant deficiency in humoral immunity that occurs in this disease. Bone radiographs typically show pure osteolytic punched-out lesions, often in association with generalized osteopenia and pathologic fractures. Bony lesions can show as expansile masses associated with spinal cord compression. Hypercalcemia caused by extensive bony involvement is common in myeloma and may dominate the clinical picture. Anemia occurs in most patients as a result of marrow infiltration and suppression of hematopoiesis and causes fatigue; granulocytopenia and thrombocytopenia are less common. Patients with myeloma are susceptible to bacterial infections because of impaired production and increased catabolism of normal immunoglobulins. Gram-negative urinary tract infections are common, as are respiratory tract infections caused by Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and Klebsiella pneumoniae. The cause of renal failure is often multifactorial; hypercalcemia, hyperuricemia, infection, and amyloid deposition can contribute. Because of their physicochemical properties, M proteins can cause a host of diverse effects, including cryoglobulinemia, hyperviscosity, amyloidosis, and clotting abnormalities resulting from interaction of the M protein with platelets or clotting factors. Most patients with myeloma exhibit symptomatic, advanced-stage disease and require therapy. Patients with asymptomatic myeloma may have an indolent course and do not always require immediate therapy. Revised international staging system for multiple myeloma: a report from International Myeloma Working Group. High-risk chromosomal abnormalities include deletion 17p and/or translocation t(4;14) and/or t(14;16). For patients with solitary bone or extramedullary plasmacytomas, particularly in the head and neck region, local radiation therapy can induce long-term remissions and is the treatment of choice. Patients with symptomatic myeloma require systemic therapy and meticulous supportive care. Although myeloma is not a curable malignancy, systemic therapy prolongs survival and dramatically improves quality of life. These agents may be used as single agents or in combinations for more intensive therapy. The novel agents are typically administered in combination with high doses of dexamethasone, which is a potent antimyeloma therapy. These agents have largely supplanted traditional chemotherapeutic agents as the cornerstone of initial and secondary therapies because they are efficacious and well tolerated. Multiple combination regimens have been devised that also incorporate chemotherapeutic agents in modest doses. The antiangiogenic properties of thalidomide subsequently led to its development as an anticancer agent. Toxicity related to thalidomide includes peripheral neuropathy, constipation, somnolence, and rash. Myelosuppression is more likely, but neuropathy and constitutional symptoms occur less frequently. Bortezomib is the first-in-class proteasome inhibitor and is an important therapy for patients with adverse cytogenetic risk factors. Bortezomib is typically administered subcutaneously and may cause thrombocytopenia, asthenia, and neuropathy. Most patients respond to initial therapy with a reduction in bone pain, hypercalcemia, and anemia in association with a decline in the M protein level. The selection of initial therapy depends on stage, cytogenetic risk, and candidacy for high-dose chemotherapy and autologous stem cell transplantation. The use of high-dose chemotherapy with alkylating agents followed by autologous peripheral stem cell infusion during first or second remission improves progression-free survival and quality of life compared with conventional therapy. Although this approach is not curative, it does represent an important treatment option for some patients and has an acceptable toxicity profile, even in older patients. Allogenic stem cell or bone marrow transplantation may be associated with durable remission in selected patients, but it carries a high nearterm risk of morbidity and mortality. Patients who experience relapse after standard therapy or transplantation may be treated with alternative chemotherapy regimens or with novel combination therapies, including newer agents and chemotherapy drugs. The first-in-class selective inhibitor of nuclear export, selinexor was recently added to the antimyeloma armamentarium for patients with relapsed or refractory disease as a fifthline therapy. Supportive care directed toward anticipated complications of myeloma is an important aspect of management. Bone resorption can be reduced with regular injections of the diphosphonates zoledronic acid or pamidronate, reducing pain and pathologic fractures. Bony lesions, particularly those involving weight-bearing bones, may require palliative irradiation for controlling pain and preventing pathologic fractures. Vertebral bony lesions may lead to spinal cord compression, with increasing back pain and neurologic symptoms. Avoidance of nephrotoxins, including intravenous contrast media, is important to prevent renal failure. Use of erythropoietin may alleviate anemia and decrease the need for blood transfusions in patients with treatment-related anemia or concomitant renal insufficiency. Multiple myeloma is considered incurable, but the overall survival of these patients has improved considerably with the use of newer agents and autologous stem cell transplantation. Patients with an adverse karyotype, including t(14;16), t(4;14), and 17p deletion, have a less favorable prognosis and are considered for more intensive therapies or clinical investigation. High-dose therapy and autologous stem cell transplantation is effective in patients with extensive disease. For a deeper discussion of these topics, please see Chapter 178, "Plasma Cell Disorders," and Chapter 179, "Amyloidosis," in Goldman-Cecil Medicine, 26th Edition. In contrast to IgG, IgM remains largely confined to the intravascular space, and as IgM levels rise, plasma viscosity increases. Epistaxis, retinal hemorrhages, dizziness, confusion, and congestive heart failure may occur as a result of the hyperviscosity syndrome. The use of fludarabine or an alkylating agent, typically employed in combination with prednisone and rituximab, is effective in decreasing adenopathy and splenomegaly and controlling the M spike but is not curative. The use of rituximab as a single agent may be complicated by initial worsening of hyperviscosity in patients with high IgM burdens. Although complete remissions are rare, patients who respond to therapy have median survivals of 4 years, and some patients survive more than a decade. Acquired disorders of lymphocyte function are far more common than congenital disorders. Patients who have undergone allogeneic organ transplantation require potent immunosuppressive drugs. Patients are treated by reducing doses of immunosuppressive drugs whenever possible. Patients with polymorphous disease early after organ transplantation may respond well to this approach. Patients who are not candidates for withdrawal of immunosuppression because of allograft rejection or who develop late monophorphic disease may respond better to treatment with rituximab alone or in combination with chemotherapy. Rare Plasma Cell Disorders Heavy-chain disease is a rare lymphoplasmacytoid neoplasm characterized by production of a defective heavy chain of the, or type. The -type heavy-chain disease is associated with lymphadenopathy, Waldeyer ring involvement with palatal edema, and constitutional symptoms. The -type heavy-chain disease, also known as Mediterranean lymphoma, is characterized by lymphoid infiltration of the small intestine with associated diarrhea and malabsorption. Congestive heart failure, bleeding diathesis, nephrotic syndrome, and peripheral neuropathy are common complications. Patients with primary amyloidosis may respond to selected treatments similar to therapy for myeloma. The combination of bortezomib, cyclophosphamide, and dexamethasone is effective in some patients. Selected patients may respond well to high-dose chemotherapy and autologous stem cell support, but there are increased risks of morbidity and mortality if significant end-organ dysfunction such as cardiomyopathy occurs. Vascular damage initiates clotting, which results in a localized platelet-fibrin plug at the site of injury to prevent blood loss. This is followed by clot containment, wound healing, eventual clot dissolution, and tissue regeneration. In healthy individuals, procoagulant and anticoagulant reactions occur continuously and in a balanced fashion so that bleeding is contained while blood vessels simultaneously remain patent to deliver adequate organ blood flow.
With increasing scores antibiotics for persistent acne buy minomycin with american express, the likelihood of a complicated antibiotic resistance of helicobacter pylori in u.s. veterans generic minomycin 50 mg visa, prolonged infection klebsiella cheap minomycin american express, and fatal outcome increases antibiotics benefits buy discount minomycin 50mg. Analgesia Despite the theoretical concern that narcotic analgesia may result in sphincter of Oddi spasm and worsening pancreatitis treatment for lower uti order minomycin pills in toronto, there is no evidence to support withholding narcotics from patients with acute pancreatitis antibiotics for uti in early pregnancy order minomycin cheap online. The physician should consider liberal use of patient-controlled analgesia, although this approach has not been compared prospectively with on-demand analgesia. Patients administered repeated doses of narcotic analgesics should have oxygen saturation monitored due to risks of unrecognized hypoxia. Prevention of complications depends largely on monitoring, vigorous hydration, and early recognition of pancreatic necrosis and choledocholithiasis. Patients with multiorgan dysfunction and those with predicted development of severe disease are at greatest risk for adverse outcomes and should be treated when possible in a care unit with intensive monitoring capability and multidisciplinary input. Nutritional Care Patients with mild acute pancreatitis can begin oral feeding within 24 hours of admission without waiting for resolution of pain or normalization of serum pancreatic enzyme levels. Early introduction of a low-fat solid diet is as safe as the traditional approach of progressive advancement from a clear liquid diet and is associated with a shorter length of hospital stay. For patients with predicted severe pancreatitis or small bowel ileus, early introduction of oral intake may not be tolerated due to postprandial abdominal pain, nausea, and vomiting. These individuals can have nutrition introduced as nasoenteric or nasogastric feeding. Nasogastric feeding offers a safe alternative to nasojejunal feeding because it appears to be equally safe and effective. Parenteral nutrition should be reserved for patients who cannot achieve sufficient caloric intake through the enteral route or those in whom enteral access cannot be maintained. Supportive Care Patients with acute pancreatitis are treated supportively with aggressive intravenous hydration, parenteral analgesics, and bowel rest. Nasogastric tube suction is indicated for symptomatic relief in patients with nausea, vomiting, and ileus. Antibiotics Antibiotic therapy is no longer recommended for patients with sterile necrosis due to the lack of proven benefit. For patients with suspected infected necrosis, appropriate antibiotics are initiated before the confirmatory diagnosis, with the initial choice taking into consideration the likely pathogenic organisms and the ability of the antimicrobials to penetrate into necrotic pancreatic tissues. After culture results are available, the antibiotics can be tailored appropriately. The risk of gallstone pancreatitis (see also Chapter 45) recurrence is as high as 50% to 75% within 6 months of the initial episode, and cholecystectomy before discharge is recommended for patients with mild attacks of pancreatitis. Cholecystectomy performed during the initial admission for patients with suspected biliary pancreatitis is associated with substantial reductions in mortality and gallstone-related complications, readmission for recurrent pancreatitis, and pancreaticobiliary complications. Cholecystectomy is often delayed in patients with severe pancreatitis to allow for better exposure of the ductal anatomy at the time of surgery. Biliary sphincterotomy leaving the gallbladder in situ is considered an effective alternative for those who are not candidates for cholecystectomy. Acute peripancreatic fluid collections do not require any specific therapy, other than supportive therapy that is standard for acute pancreatitis. Most remain sterile and are reabsorbed spontaneously during the first several weeks after the onset of acute pancreatitis. When a localized acute peripancreatic fluid collection persists beyond 4 weeks, it is likely to develop into a pancreatic pseudocyst. While patients with asymptomatic pseudocysts should be followed, for those who are symptomatic, pseudocyst drainage should be considered. Indications for pseudocyst drainage include suspicion of infection or progressive Fluid Management Vigorous fluid resuscitation is important for maintaining the microcirculation and perfusion of the pancreas during the early phase of acute pancreatitis. Early aggressive intravenous hydration during the first 12 to 24 hours after the onset of symptoms translates into a potential benefit of reduced pancreatic necrosis and organ failure. Crystalloid, the preferred intravenous fluid, is administered at an initial rate of 250 to 500 mL/ hour or 5 to 10 mL/kg/hr with a preceding bolus infusion for individuals with severe volume depletion. Goal-directed therapy is defined as titration of intravenous fluids every few hours to specific clinical and biochemical targets of perfusion. Antibiotic use, including the type and duration of treatment, continues to be examined, and these suggested approaches will likely be modified by the findings of future studies. In symptomatic patients, if the pseudocyst is mature and encapsulated, treatment can involve endoscopic, surgical, or percutaneous drainage. Sterile pancreatic necrosis usually is treated with supportive medical care during the first several weeks, even in patients with multiple organ failure. After the acute pancreatic inflammatory process has subsided and coalesced into an encapsulated structure. Asymptomatic pancreatic necrosis does not warrant intervention, regardless of the extent and location. The development of infection in the necrotic collection is the main indication for therapy. The development of fever leukocytosis and increasing abdominal pain suggests infection of the necrotic tissue. The consensus is that the best outcomes are achieved when invasive interventions are delayed for a minimum of 4 weeks after the onset of disease to allow liquefaction of necrotic tissues and a fibrous rim to form around the necrosis. Patients with infected necrosis are initially treated with broad-spectrum antibiotics and medical support to allow encapsulation of the necrotic collections, which may facilitate intervention and reduce complications of bleeding and perforation. When there is dramatic clinical deterioration, patients are not stable and delay is not feasible, and early intervention with a percutaneous drain is required. Traditional management of infected pancreatic necrosis has been open surgical necrosectomy with closed irrigation by indwelling catheters, necrosectomy with closed drainage without irrigation, or necrosectomy and open packing. The open surgical approaches are associated with a high morbidity (34% to 95%) and mortality (11% to 39%) rates. A more conservative step-up approach using percutaneous catheter drainage as the initial treatment has gained favor, and a delay in invasive treatment is now standard. This approach is superior to traditional open necrosectomy with respect to the risk of major complications or death. The two conditions may overlap because recurrent attacks of acute pancreatitis may lead to chronic pancreatitis, and individuals with chronic pancreatitis may experience exacerbations of acute pancreatitis. The annual incidence of chronic pancreatitis ranges from 5 to 12 cases per 100,000 people, and the prevalence is about 50 cases per 100,000 people. The most common cause of chronic pancreatitis is chronic alcoholism, accounting for 45% to 65% of cases. Alcohol can cause episodes of acute pancreatitis, but at the time of the initial attack, structural and functional abnormalities often indicate underlying chronic pancreatitis. Because most alcohol users do not develop pancreatitis, the presumption is that unidentified genetic, dietary, or environmental influences must coexist with alcohol use. The effect of smoking is synergistic with alcohol consumption and contributes profoundly to the development and progression of the disease. Gallstone pancreatitis, the major cause of acute pancreatitis, rarely leads to chronic pancreatitis. Occasionally, patients exhibit exocrine or endocrine insufficiency in the absence of pain. Other patients are asymptomatic and are found to have chronic pancreatitis incidentally on imaging. The pain of chronic pancreatitis is typically epigastric, often radiates to the back, is occasionally associated with nausea and vomiting, and may be partially relieved by sitting upright or leaning forward. Early in the course of chronic pancreatitis, the pain may occur in discrete attacks; as the condition progresses, the pain tends to become continuous. Possible causes include inflammation of the pancreas, increased intrapancreatic pressure, neural inflammation, and extrapancreatic causes, such as stenosis of the common bile duct and duodenum. Glucose intolerance occurs with some frequency in chronic pancreatitis, but overt diabetes mellitus usually manifests late in the course of disease. Diabetes in patients with chronic pancreatitis is different from typical type 1 diabetes in that the pancreatic alpha cells, which produce glucagon, are also affected, increasing the risk of hypoglycemia. Steatorrhea usually occurs before protein deficiencies because lipolytic activity decreases faster than proteolysis. Because reduced vitamin D absorption can result in osteoporosis, osteopenia, and fractures, periodic assessment of vitamin D levels and bone densitometry are recommended. Clinicians have preferentially relied on noninvasive methods to circumvent the challenges associated with direct pancreatic function tests. Clinically available indirect tests of pancreatic function include analyses of fecal fat, fecal elastase, and serum trypsin. This test is primarily performed for patients with suspected chronic pancreatitis who have chronic abdominal pain but negative or equivocal results of imaging studies. The secretin stimulation test has been infrequently used in clinical practice because the study is labor intensive and is associated with discomfort. Endoscopic collection methods have simplified pancreatic fluid collection and made the test more suitable for clinical use. The 72-hour fecal fat determination is sometimes used for detection of steatorrhea (fecal fat >7 g/24 hours), but the test is not specific for pancreatic exocrine insufficiency. The test also lacks sensitivity because steatorrhea occurs only in advanced chronic pancreatitis. Because the quantitative fecal fat test is inconvenient, unpleasant for patients, and prone to laboratory error, a qualitative assay is used preferentially in clinical practice to assess for malabsorption. Determination of fecal elastase is the most commonly used noninvasive indirect test for the diagnosis of pancreatic exocrine insufficiency. Elastase, a protease synthesized by pancreatic acinar cells, is useful for evaluating insufficiency because it is stable in stool, unaffected by pancreatic enzyme replacement, and correlates well with stimulated pancreatic function test results. Moderate to severe exocrine insufficiency is based on fecal elastase values of less than 200 g/g of stool. False-positive results can be seen with diarrheal illnesses, due to a dilutional effect. In early chronic pancreatitis, however, mild abnormalities of pancreatic function can precede the morphologic changes seen on imaging. Studies of pancreatic structure may remain normal even with advanced deterioration of pancreatic function. Laboratory evaluations of serum pancreatic enzymes, such as amylase and lipase, are frequently normal in the setting of well-established chronic pancreatitis, even during painful exacerbations. Indirect tests measure the consequences of pancreatic insufficiency, and although more widely available, the results usually are not abnormal until enzyme output has declined by more than 90%. Abstention may decrease the frequency of painful attacks and reduce the likelihood of pancreatic function deterioration and development of pancreatic cancer. Nonopioid analgesics such as acetaminophen and nonsteroidal anti-inflammatory drugs are used as initial treatment. If possible, the use of opioids should be avoided due to the risk of abuse, tolerance, and addiction. The risk of dependence to opioids is not known in this setting; however, patients with previous addictive behaviors such as substance use with alcohol or tobacco are at greater risk for analgesic dependence and addiction. Oral pancreatic enzyme replacement, somatostatin analogue, and enteral nutrition are proposed treatments to blunt pain by reducing pancreatic secretion. These therapies are of unproven benefit and not routinely recommended as adjuncts to pain therapy. Gabapentinoids, including pregabalin, have been used effectively to treat neuropathic pain disorders, including diabetic neuropathy and neuropathic pain of central origin. Based on the finding that pancreatic pain is accompanied by similar alterations of central pain processing, studies suggest a benefit with pregabalin as an adjuvant treatment to decrease pain associated with chronic pancreatitis. Similarly, tricyclic antidepressants, selective serotonin reuptake inhibitors, and serotonin-norepinephrine reuptake inhibitors can be administered on a trial basis. Neuroablative techniques such as celiac plexus blockade can be performed by injection of a local anesthetic and a steroid into the region of the celiac ganglia. The results are disappointing with a pain reduction in a minority of individuals (15% to 50%) that is not durable with pain reduction or relief of up to 1 to 6 months. Oxidative stress can cause direct pancreatic acinar cell damage through several pathways. Supplementation with antioxidants, such as selenium, vitamins C and E, and methionine, may relieve pain and reduce oxidative stress. In a randomized trial, the reduction in the number of painful days per month was higher for the patients who received antioxidants compared with those who received placebo (7. Patients who received antioxidants also were more likely to become pain free (32% vs. Endoscopic decompression of the pancreatic duct is an option for obstruction caused by strictures, stones, or sphincter of Oddi dysfunction. Endoscopic therapies include pancreatic sphincterotomy, stricture dilation, stone with a sensitivity for the diagnosis of chronic pancreatitis of 71% to 93% and a specificity of 89% to 100%.
Buy cheap minomycin 100 mg. Salamat Dok: Antibiotic-Resistant Gonorrhea | Discussion.


















