Colchicine

Michael A. Tall, MD
- Chief, Magnetic Resonance Imaging
- Wilford Hall Medical Center
- Lackland AFB, Texas
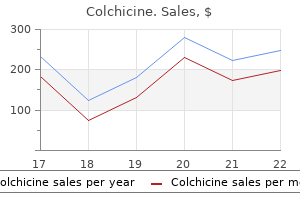
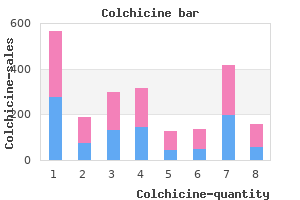
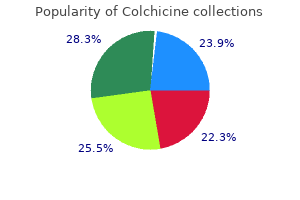
Unlike stents deployed to treat most descending thoracic aortic aneurysms antibiotics for uti flucloxacillin buy colchicine without a prescription, stents deployed to treat descending aortic dissections must not be ballooned antibiotics japan purchase cheapest colchicine, because ballooning can cause a new intimal tear infection japanese movie order colchicine online from canada, retrograde dissection into the ascending aorta 5th infection colchicine 0.5 mg without a prescription, or even aortic rupture antibiotic resistant outbreak buy 0.5 mg colchicine fast delivery. Chronic Dissection Endovascular treatment of chronic descending aortic dissection is also controversial and remains under investigation antibiotic quick reference guide colchicine 0.5 mg generic. Furthermore, interfering with false lumen perfusion may cause ischemic complications, such as bowel infarction or renal failure. Until the safety and effectiveness of endovascular repair for this condition have been demonstrated, patients with chronic descending aortic dissection should be treated with conventional nonoperative management until indications for open surgical repair develop. Covering the focal ulceration with a stent graft has been shown to be an effective treatment. Open Repair Acute Dissection In patients with acute aortic dissection, sur- gical repair of the descending thoracic or thoracoabdominal aorta is traditionally associated with high morbidity and mortality. Because the most common site of rupture in descending aortic dissection is in the proximal third of the descending thoracic aorta, the upper half of the descending thoracic aorta is usually repaired. Graft replacement of the entire thoracoabdominal aorta is not attempted in such cases unless a large coexisting aneurysm mandates this radical approach. Similarly, the repair is not extended into the aortic arch unless the arch is aneurysmal, even if the primary tear is located there. Patients with chronic dissection who require emergency repair because of acute pain or rupture also undergo limited graft replacement of the symptomatic segment. Because repairing acute dissections entails an increased risk of paraplegia, adjuncts that provide spinal cord protection, such as cerebrospinal fluid drainage and left heart bypass, are used liberally during such repairs,180 even if the repair is confined to the upper descending thoracic aorta. Proximal control usually is obtained between the left common carotid and left subclavian arteries; any mediastinal hematoma near the proximal descending thoracic aorta is avoided until proximal control is established. After the aorta is opened, the dissecting membrane is excised from the section undergoing graft replacement. The proximal and distal anastomoses use all layers of the aortic wall, thereby excluding the false lumen in the suture lines and directing all blood flow into the true lumen. Although the relative lack of mural thrombus ensures the presence of multiple patent intercostal arteries, extreme tissue fragility may preclude their reattachment. Malperfusion Syndrome Lower-extremity ischemia is commonly addressed with surgical extra-anatomic revascularization techniques, such as femoral-to-femoral bypass grafting. In patients with abdominal organ ischemia, flow to the compromised bed must be re-established swiftly. When an endovascular approach is unavailable or unsuccessful, open surgery is necessary. Although they are considered second-line therapies, multiple techniques are available, including graft replacement of the aorta (with flow redirected into the true lumen), open aortic fenestration, and visceral or renal artery bypass. Chronic Dissection A more aggressive replacement usually is performed during elective aortic repairs in patients with chronic dissection. One key difference is the need to excise as much dissecting membrane as possible to clearly identify the true and false lumens and to locate all important branch vessels. When the dissection extends into the visceral or renal arteries, the membrane can be fenestrated, or the false lumen can be obliterated with sutures or intraluminal stents. Asymmetric expansion of the false lumen can create wide separation of the renal arteries. This problem is addressed by reattaching the mobilized left renal artery to a separate opening in the graft or by performing a left renal artery bypass with a side graft. Wedges of dissecting membrane also are excised from the aorta adjacent to the proximal and distal anastomoses, which allows blood to flow through both true and false lumens. When placing the proximal clamp is not technically feasible, hypothermic circulatory arrest can be used to facilitate the proximal portion of the repair. When performed in specialized centers, these operations are associated with excellent survival rates and acceptable morbidity rates. The interpretation of outcomes data is complicated by site-specific variables, such as the number of years reported and whether data are taken from single-practice centers or from pooled, multicenter, or national registries, and by patient-specific variables, such as type of enrollment, urgency and extent of repair, concomitant procedures performed, and the presence of preexisting risk factors such as advanced age, previous cardiovascular repair, disease of any system or organ, or connective tissue disorder. Repair of Proximal Aortic Aneurysms 817 Risks associated with the open repair of the proximal aorta vary by extent of repair and are greatest for repairs involving total arch replacement. All varieties of aortic root replacement have shown acceptable early mortality rates and few complications. The patient has previously undergone composite valve graft replacement of the aortic root and ascending aorta. After left heart bypass is initiated, the proximal portion of the aneurysm is isolated by placing clamps on the left subclavian artery, between the left common carotid and left subclavian arteries, and across the middle descending thoracic aorta. The dissecting membrane is excised, and bleeding intercostal arteries are oversewn. The aorta is prepared for proximal anastomosis by transecting it distal to the proximal clamp and separating this portion from the esophagus (not shown). The proximal anastomosis between the aorta and an appropriately sized Dacron graft is completed with continuous polypropylene suture. After left heart bypass has been stopped and the distal aortic cannula has been removed, the proximal clamp is repositioned onto the graft, the other two clamps are removed, and the remainder of the aneurysm is opened. The rest of the dissecting membrane is excised, and the openings to the celiac, superior mesenteric, and renal arteries are identified. Selective visceral perfusion with oxygenated blood from the bypass circuit is delivered through balloon perfusion catheters placed in the celiac and superior mesenteric arterial ostia. To minimize spinal cord ischemia, the proximal clamp is repositioned distal to the intercostal reattachment site. Selective perfusion of the visceral arteries continues during their reattachment to the graft. After the balloon perfusion catheters are removed and the visceral anastomosis is completed, the clamp is again moved distally, restoring blood flow to the celiac, renal, and superior mesenteric arteries. Even though these patients had substantial comorbidity and 83% underwent concomitant cardiac repairs, acceptable rates of early mortality (11%) and stroke (6%) were obtained. Other studies indicate that the enhanced risk of neurocognitive disturbances in ascending repairs using circulatory arrest are not offset by lower rates of early mortality. For example, by adopting contemporary approaches, we have reduced early mortality for stage 1 elephant trunk repairs from 12% to 2% in our patients. Other contemporary reports of the use of techniques such as moderate hypothermia and Y-graft approaches201-204 indicate similarly improved outcomes; early mortality ranges from 1% to 7%, stroke rates range from 1% to 6%, and no cases of paraplegia are reported. Although paraplegia has traditionally been an unusual and infrequent complication of aortic arch repair, it has been reported as a complication of "long" elephant trunk approaches205 and frozen elephant trunk approaches. A metaanalysis conducted by Koullias and Wheatley82 of data from 15 studies with 463 patients found an average 30-day mortality rate of 8. Of note, relatively few repairs (30%) were performed "off-pump," and the majority of repairs used cardiopulmonary bypass or hypothermic circulatory arrest. Additionally, several reports of small series (ranging from 33 to 66 patients) have documented a substantial risk of acute retrograde aortic dissection during hybrid arch repairs; rates range from 3. This registry was established in 1996 and has accumulated data from >3000 patients treated for acute aortic dissection at 30 centers in 11 countries. Thus, at present, the use of stent grafts to treat chronic descending aortic dissection should be considered experimental. Contemporary results of open repairs of descending thoracic aortic aneurysms, including those performed in select patients with chronic dissection, indicate that early mortality rates range from 4. Several studies have compared endovascular and surgical approaches to descending thoracic aortic repair. Some studies found no significant differences in rates of early death, stroke, and paraplegia,217,226,227 whereas others found that surgical patients had higher rates of early mortality (27%)228 and paraplegia (14%). Of note, 40% of these patients Repair of Distal Aortic Aneurysms Endovascular Repair of Descending Thoracic Aortic Aneurysms. In the earliest series of endovascular repairs of descending thoracic aortic aneurysms, mortality and morbidity were difficult to assess. Most of the reported series were small and included a large proportion of high-risk patients with substantial comorbidity. However, 62 patients (60%) were not considered candidates for thoracotomy and open surgical repair; as expected, this group experienced the majority of the morbidity and mortality. Evidence from pivotal, nonrandomized trials that compared patients who underwent endograft exclusion with historical or concurrent patients who underwent open repair215-217 shows that the stent graft groups had significantly less morbidity and early mortality than the open repair groups, although in two of the trials, a nonsignificant between-group difference 820 were treated at centers averaging only one thoracoabdominal aortic aneurysm repair per year. Another study found that, of patients who survived surgical treatment of acute descending aortic dissection, approximately 96% were alive at 1 year and approximately 83% were alive at 3 years after the procedure,239 which is substantially better than 1-year survival after endovascular repair in acute complicated distal dissection. The availability and development of adjuncts and endovascular techniques have supported the constant evolution of surgical strategies to tackle these complex problems. Repair strategies range from isolated, totally endovascular aortic repair for descending thoracic aneurysms to extensive total aortic and staged replacements with a combination of both open and endovascular techniques. Regardless of the difficulty of accurately assessing the risks associated with aortic repair, surgical repair of the thoracoabdominal aorta clearly remains the most challenging aortic repair in terms of mortality and morbidity. Risk factors associated with treatment failure- defined as death or need for surgery-include an enlarged aorta, persistent hypertension despite maximal treatment, oliguria, and peripheral ischemia. Among patients who receive nonoperative treatment for descending aortic dissection and who survive the acute period, approximately 90% remain alive 1 year later, and approximately 76% are alive 3 years later. For malperfusion of the visceral or renal arteries, an endovascular approach is ideal. The Stanford group reported a 93% technical success rate for endovascular reperfusion of an ischemic bed. The early mortality rate was 16%, comparable to that associated with open techniques. However, patients with complicated acute descending dissection remain susceptible to late events; at 1 year, survival is approximately 70%, and reintervention is needed in about 10% of survivors. We recently reported our contemporary experience with 32 patients with acute complicated descending aortic dissection, including 7 patients (22%) with aortic rupture. Complexities included dangerously large aneurysms in the majority of patients (69%), which implied either rapid expansion or an aneurysm superimposed on the dissection. Malperfusion was present in one patient; this patient had an open fenestration procedure. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. Filamin A mutations cause periventricular heterotopia with Ehlers-Danlos syndrome. Bicuspid aortic valves are associated with aortic dilatation out of proportion to coexistent valvular lesions. Aortic dimensions in patients with bicuspid aortic valve without significant valve dysfunction. Aortic root dilatation in young men with normally functioning bicuspid aortic valves. Congenitally bicuspid aortic valves: a surgical pathology study of 542 cases (1991 through 1996) and a literature review of 2,715 additional cases. Matrix metalloproteinases in ascending aortic aneurysms: bicuspid versus trileaflet aortic valves. Vascular matrix remodeling in patients with bicuspid aortic valve malformations: implications for aortic dilatation. Tissue microarray detection of matrix metalloproteinases, in diseased tricuspid and bicuspid aortic valves with or without pathology of the ascending aorta. Evidence in favor of linkage to human chromosomal regions 18q, 5q, and 13q for bicuspid aortic valve and associated cardiovascular malformations. Failure to prevent progressive dilation of ascending aorta by aortic valve replacement in patients with bicuspid aortic valve: comparison with tricuspid aortic valve. Bacteriologic and surgical determinants of survival in patients with mycotic aneurysms. Natural history of thoracic aortic aneurysms: indications for surgery, and surgical versus nonsurgical risks. Yearly rupture or dissection rates for thoracic aortic aneurysms: simple prediction based on size. Aortic dissection after aortic valve replacement: incidence and consequences for strategy. Risk of late aortic events after an isolated aortic valve replacement for bicuspid aortic valve stenosis with concomitant ascending aortic dilation. Utility of transesophageal echocardiography in the diagnosis of disease of the thoracic aorta. Prevention of contrastinduced nephropathy with sodium bicarbonate: a randomized controlled trial. Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. Superior nationwide outcomes of endovascular versus open repair for isolated descending thoracic aortic aneurysm in 11,669 patients. Practice patterns for thoracic aneurysms in the stent graft era: health care system implications. Endovascular versus open repair of ruptured descending thoracic aortic aneurysms: a nationwide risk-adjusted study of 923 patients. Thoracic or thoracoabdominal approaches to endovascular device removal and open aortic repair. Estimating group mortality and paraplegia rates after thoracoabdominal aortic aneurysm repair. A new predictive model for adverse outcomes after elective thoracoabdominal aortic aneurysm repair. Aortic root replacement with a new stentless aortic valve xenograft conduit: preliminary hemodynamic and clinical results.
As portal venous pressure increases virus in us purchase colchicine 0.5mg amex, however antibiotic resistance global buy generic colchicine 0.5mg online, the collateral communications with the systemic circulation dilate antimicrobial yoga pant colchicine 0.5 mg generic, and a large amount of blood may be shunted around the liver and into the systemic circulation virus 68 symptoms 2014 order colchicine in united states online. An understanding of portal vein patency and anatomy is crucial before undertaking portosystemic shunts virus living purchase colchicine 0.5mg mastercard, hepatic resection antibiotic resistant bacteria cheap 0.5mg colchicine fast delivery, or hepatic transplantation. Doppler ultrasound is capable of outlining the anatomy of the portal vein, excluding the presence of thrombosis, and identifying the direction of portal venous blood flow. Visceral angiography and portal venography are reserved for cases that cannot be evaluated satisfactorily by noninvasive methods and require further clarification of portal patency or anatomy. The most accurate method of determining portal hypertension is hepatic venography. Ascites occurs in the setting of severe portal hypertension in combination with hepatocyte dysfunction. The umbilical vein may recannulate and dilate, leading to visible collaterals on the abdominal wall. Anorectal varices are present in approximately 45% of cirrhotic patients and must be distinguished from hemorrhoids, which do not communicate with the portal system and are not present at increased incidence in patients with portal hypertension. Intra-abdominal venous flow pathways leading to engorged veins (varices) from portal hypertension. Etiology and Clinical Features of Portal Hypertension Management of Gastroesophageal Varices the causes of portal hypertension can be divided into three major groups: presinusoidal, sinusoidal, and postsinusoidal. The most significant clinical finding associated with portal hypertension is the development of gastroesophageal varices, which are mainly supplied by the anterior branch of the left gastric (coronary) vein. Portal hypertension also results in splenomegaly with enlarged, tortuous, and even aneurysmal splenic vessels. Splenomegaly is frequently associated with functional hypersplenism, the most significant manifestation and the leading cause of morbidity and mortality related to portal hypertension is variceal bleeding. Approximately 30% of patients with compensated cirrhosis and 60% of patients with decompensated cirrhosis have esophageal varices. If left untreated, 70% of patients who survive the initial bleed will experience recurrent variceal hemorrhage within 2 years of the index hemorrhage. Prevention of Variceal Bleeding Current measures aimed at preventing variceal bleeding include the administration of nonselective -blockers and prophylactic 1282 endoscopic surveillance with variceal band ligation. Meta-analyses have demonstrated that nonselective -blockers such as propranolol and nadolol reduce the index variceal bleed by approximately 45% and decrease bleeding mortality by 50%. Endoscopic surveillance with prophylactic variceal band ligation has been associated with a lower incidence of a first variceal bleed. The needle track is dilated until a portal pressure gradient of 12 mmHg is achieved. A high rate of thrombosis is seen and can be attributed to intimal hyperplasia of the metallic stent. Blood resuscitation should be performed carefully to reach a hemoglobin level of approximately 8 g/dL. Overzealous replacement of blood products and administration of saline can lead to both rebleeding and increased mortality. Administration of fresh frozen plasma and platelets can be considered in patients with severe coagulopathy. Cirrhotic patients with variceal bleeding have a high risk of developing bacterial infections, which are associated with increased risks of rebleeding and mortality. Spontaneous bacterial peritonitis accounts for approximately half of these infections, with urinary tract infections and pneumonias comprising the remainder. Vasoactive medications decrease blood flow to the gastroesophageal varices and can be initiated as soon as the diagnosis of variceal bleeding is made. Although vasopressin is the most potent available vasoconstrictor, its use is limited by its systemic vasoconstrictive effects that can produce hypertension, myocardial ischemia, arrhythmias, ischemic abdominal pain, and limb gangrene. Octreotide, a somatostatin analog, has the advantage that it can be administered for 5 days or longer, and it is currently the preferred pharmacologic agent for initial management of acute variceal bleeding. In addition to pharmacologic therapy, endoscopy with variceal band ligation should be carried out as soon as possible. This combination of pharmacologic and endoscopic therapy has been shown both to 6 improve the initial control of bleeding and to increase the 5-day hemostasis rate. Using a transjugular or transfemoral approach, a balloon-occlusion catheter is directed through the left renal vein into the spontaneous shunt, which is then obliterated with the use of a sclerosing agent. The occlusion of spontaneous shunts, however, can theoretically exacerbate portal hypertension, precipitate hemorrhage from esophageal varices, and exacerbate the accumulation of ascites. Surgical Shunting Luminal Tamponade When medical and endoscopic measures fail to control variceal hemorrhage, balloon tamponade using a Sengstaken-Blakemore tube will control refractory bleeding in up to 90% of patients. However, its application is limited due to the potential for complications, which include aspiration, airway obstruction, and esophageal perforation due to overinflation or pressure necrosis. Therefore, the use of a Sengstaken-Blakemore tube should not exceed 36 hours to avoid tissue necrosis, and this treatment modality should only be considered a temporary bridge to more definitive measures of variceal hemorrhage control. The aim of the surgical shunt is to reduce portal venous pressure, maintain total hepatic and portal blood flow, and avoid the high incidence of complicating hepatic encephalopathy. Currently this shunt is rarely performed due to the high incidence of hepatic encephalopathy and decreased liver function resulting from the reduction of portal perfusion. The Eck fistula also makes subsequent hepatic transplantation much more technically difficult. The mesocaval shunt is technically easier to perform and can be easily ligated during subsequent hepatic transplantation. The smaller caliber of the shunt avoids the deleterious effects of portal blood flow deprivation on hepatic function. Small-diameter portosystemic shunts have been reported to reduce the incidence of encephalopathy but at the expense of increased risks of shunt thrombosis and rebleeding. It requires division of the gastroesophageal collaterals and allows venous drainage of the stomach and lower esophagus through the short gastrosplenic veins into the spleen, and ultimately decompresses the left upper quadrant by allowing the splenic vein to drain directly into the left renal vein via an end-to-side splenic to left renal vein anastomosis. This shunt has the advantages of being associated with a lower rate of hepatic encephalopathy and decompensation and not interfering with subsequent liver transplantation. Nonshunt Surgical Management of Refractory Variceal Bleeding In the patient with extrahepatic portal vein thrombosis and refractory variceal bleeding, the Sugiura procedure may be considered. The Sugiura procedure consists of extensive devascularization of the stomach and distal esophagus along with transection of the esophagus, splenectomy, truncal vagotomy, and pyloroplasty. As with performance of surgical shunts, patient survival is dependent on hepatic reserve at the time of the surgical procedure. Experience in Western countries is somewhat limited, and a number of modifications have been made to the original Sugiura procedure over time. Hepatic Transplantation Patients with cirrhosis, portal hypertension, and variceal bleeding usually die as a result of hepatic failure and not acute blood loss. Hepatic transplantation also can be considered for the patient with variceal bleeding refractory to all other forms of management. Previous creation of an Eck fistula, however, does make hepatic transplantation much more technically difficult, and therefore this procedure should be avoided in the transplant candidate. Activated protein C resistance, generally related to factor V Leiden mutation, is present in approximately 25% of patients. The obstruction results in hepatomegaly, liver congestion, and right upper quadrant pain. In addition, liver perfusion via the portal vein may be decreased, and 70% of affected patients have noninflammatory centrilobular necrosis on biopsy. Budd-Chiari Syndrome 1284 Abdominal ultrasonography is the initial investigation of choice and can demonstrate the absence of hepatic vein flow, spider web hepatic veins, and collateral hepatic veins. Initial treatment consists of diagnosing and medically managing the underlying disease process and preventing extension of the hepatic vein thrombosis through systemic anticoagulation. Radiologic and surgical intervention should be reserved for patients whose condition is nonresponsive to medical therapy. Surgical shunting, namely with the side-to-side portacaval shunt, essentially turns the portal vein into a hepatic outflow tract. Most patients with a portacaval shunt show improvement in hepatic function and fibrosis at 1 year without significant hepatic encephalopathy. Due to the high level of reticuloendothelial cells in the liver, nonviral infections are unusual. Pyogenic liver abscesses are the most common liver abscesses seen in the United States. They may be single or multiple and are more frequently found in the right lobe of the liver. Approximately 40% of abscesses are monomicrobial, an additional 40% are polymicrobial, and 20% are culture-negative. The most common infecting agents are gram-negative bacteria; Escherichia coli is found in two thirds of cases, and other common organisms include Streptococcus faecalis, Klebsiella, and Proteus vulgaris. In patients with endocarditis and infected indwelling catheters, Staphylococcus and Streptococcus species are more commonly found. In the past, pyogenic liver abscesses often resulted from infections of the intestinal tract such as acute appendicitis and diverticulitis, which then spread to the liver via the portal circulation. With improved imaging modalities and earlier diagnosis of these intra-abdominal infections, this particular etiology of pyogenic liver abscesses has become less common. A thorough history and physical examination are usually helpful in identifying the underlying cause of the liver abscess. Significant abnormalities in the results of the remaining liver function tests are unusual. Blood cultures will only reveal the causative organism in approximately 50% of cases. Ultrasound examination of the liver reveals pyogenic abscesses as round or oval hypoechoic lesions with well-defined borders and a variable number of internal echoes. Empiric antibiotic therapy should cover gram-negative and anaerobic organisms; percutaneous needle aspiration and culture of the aspirate may be useful in guiding subsequent antibiotic therapy. Placement of a percutaneous drainage catheter is beneficial only for a minority of patients, as most pyogenic abscesses are quite viscous and catheter drainage is often ineffective. Surgical drainage either via the laparoscopic or open approach may become necessary if initial therapies fail. Anatomic surgical resection can be performed in patients with recalcitrant abscesses. It must be kept in mind throughout the evaluation and treatment of the presumed pyogenic abscess that a necrotic hepatic malignancy must not be mistaken for a hepatic abscess. Multiple hepatic abscesses are seen in a patient after an episode of diverticulitis. Note the loculated large central abscess as well as the left lateral segment abscess. Amebiasis is most common in subtropical climates, especially in areas with poor sanitation. The cystic form passes through the stomach and small bowel unharmed and then transforms into a trophozoite in the colon. Here it invades the colonic mucosa forming typical flask-shaped ulcers, enters the portal venous system, and is carried to the liver. Occasionally, the trophozoite will pass through the hepatic sinusoid and into the systemic circulation, which results in lung and brain abscesses. Amebae multiply and block small intrahepatic portal radicles with consequent focal infarction of hepatocytes. The amebic abscess is most commonly located in the superior-anterior aspect of the right lobe of the liver near the diaphragm and has a necrotic central portion that contains a thick, reddish brown, pus-like material. Amebiasis should be considered in patients who have traveled to an endemic area and present with right upper quadrant pain, fever, hepatomegaly, and hepatic abscess. Even though this disease process is secondary to a colonic infection, the presence of diarrhea is unusual. This serologic test has a high sensitivity, and therefore amebiasis is unlikely if the test results are negative. Metronidazole 750 mg three times a day for 7 to 10 days is the treatment of choice and is successful in 95% of cases. Defervescence usually occurs in 3 to 5 days, but the time necessary for the abscess to resolve depends on the initial size at presentation and varies from 30 to 300 days. Aspiration of the abscess rarely is needed and should be reserved for patients with large abscesses, those who do not respond to medical therapy, or those who appear to be superinfected. Furthermore, abscesses of the left lobe of the liver at risk for rupture into the pericardium should be treated with aspiration and drainage. Hydatid Disease Hydatid disease is due to infection by the tapeworm Echinococcus granulosus in its larval or cyst stage. Scolices, contained in the cysts, adhere to the small intestine of dogs and become adult taenia, which attach to the intestinal wall. The infected ova-containing feces of dogs contaminate grass and farmland, and the ova are ingested by intermediate hosts such as sheep, cattle, pigs, and humans. The liberated ovum then burrows through the intestinal mucosa and is carried by the portal vein to the liver, where it develops into an adult cyst. Most cysts are caught in the hepatic sinusoids, and therefore 70% of hydatid cysts form in the liver. A few ova pass through the liver and are held up in the pulmonary capillary bed or enter the systemic circulation, forming cysts in the lung, spleen, brain, or bones. Hydatid disease is most common in sheep-raising areas, where dogs have access to infected offal. These include South Australia, New Zealand, Africa, Greece, Spain, and the Middle East. Hydatid cysts commonly involve the right lobe of the liver, usually the anterior-inferior or posterior-inferior segments.
Buy colchicine with mastercard. Antimicrobial Stewardship: Ireland’s strategy to combat antimicrobial resistance.
Hypertension antibiotics for uti in 3 year old discount 0.5mg colchicine mastercard, a component of the metabolic syndrome antibiotic ointment for babies cheap 0.5mg colchicine with visa, is one of the cardiovascular diseases that are increased in the setting of obesity antibiotics for sinus infection and breastfeeding generic 0.5mg colchicine. Elevated arterial pressure in patients with obesity-related hypertension is associated with increased cardiac output and total peripheral resistance antimicrobial keyboard cover purchase 0.5mg colchicine. The elevated output is related to expanded intravascular volume that increases cardiopulmonary volume antibiotics for acne how long discount 0.5 mg colchicine with amex, venous return antibiotics for dogs ear infection uk order colchicine 0.5 mg otc, and left ventricular preload; the elevated pressure and total peripheral resistance increase afterload. This dual ventricular overload promotes a dimorphic, concentric, and eccentric hypertrophy in response to the volume and pressure overload. Increased myocardial oxygen demand results from the elevated tension in the left ventricular wall, reflecting its increased diameter and pressure, and provides a physiologic rationale for the greater potential of coronary arterial insufficiency and cardiac failure. There is greater renal blood flow and lower renal vascular resistance in patients with obesity-related hypertension at any level of arterial pressure. This may be offset by an increased renal filtration fraction that may favor protein deposition and glomerulosclerosis. These manifestations occur after all the various bariatric operations that produce weight loss. Much of the risk is secondary to the processes mentioned earlier, which produce hypertension and cardiac hypertrophy. Hypertension and obesity have significant independent associations with left ventricular hypertrophy and cardiac wall thickness. Obesity is particularly strongly associated with left ventricular internal diameter. A recent systematic review of long-term cardiovascular risk factor reduction after bariatric surgery involved 73 studies and 19,543 subjects with a mean age of 42 years; 76% of subjects were female, and 44%, 24%, and 44% had a baseline hypertension, diabetes, and hyperlipidemia, respectively. Echocardiographic results from 713 subjects showed statistically significant improvements in left ventricular mass, E/A ratio, and isovolumic relaxation time postoperatively. Thus far, there are no long-term randomized controlled trials comparing bariatric surgery with nonsurgical medical treatment of obesity that evaluate cardiovascular endpoints and mortality. However, 12 cohort-matched studies comparing bariatric surgery with nonsurgical controls have recently been reviewed. Bariatric surgery can produce resolution of many, if not all, of the comorbid medical problems associated with obesity and present at the time of surgery. This is true to some extent for all bariatric procedures, although some are more efficient at reversing specific comorbid problems than others. The recurrence of symptoms is higher, likely due to a higher incidence of wrap herniation into the mediastinum and other mechanical failure of the fundoplication, which in turn is likely affected by the increased intra-abdominal pressure of the obese condition. In one recent study of 349 patients considering bariatric surgery who were referred and tested, only 17% had no sleep apnea, whereas 32% had mild, 18% moderate, and 33% severe sleep apnea. Of 83 patients using continuous positive airway pressure or bilevel positive airway pressure preoperatively, only 31 still required it, and they had decreased setting requirements. A recent systematic review of 13,900 patients (69 studies) showed significant improvement or resolution of sleep apnea in more than 75% of bariatric surgery patients. The findings suggested that much of the improvement achieved was in the mild to moderate weight loss range, with little benefit of further weight loss. Dixon and colleagues181 studied 23 asthmatic patients who underwent bariatric surgery and found a significant improvement in asthma control. Boulet and colleagues182 found similar results in their cohort of 12 patients with asthma who experienced significant weight loss after bariatric surgery. The disease is a spectrum of liver abnormalities including steatosis, steatohepatitis, fibrosis, and cirrhosis of the liver. However, since the treatment of the disease is weight loss, patients with mild forms of the disease need no further treatment or follow-up. Biopsy reports showing any degree of fibrosis should be further followed up by a hepatologist. A recent systematic review of the available literature found many retrospective and prospective observational cohort studies, but no randomized control trials or case-control series. Musculoskeletal problems, especially degenerative joint disease and low back pain, are among the most common complaints and associated comorbid problems of the severely obese population. Quantitation of their severity, however, is often difficult, making resolution or improvement equally difficult. Symptoms often resolve and usually improve in patients who experience significant weight loss. This is likely a combined effect of the direct lessened work load as well as some secondary resolution of the inflammatory process of the joints brought on directly and indirectly by obesity. Patients with osteoarthritis of the neck, shoulder, spine, hip, knee, ankle, wrist, and hand have been shown to have improved or resolved joint pain after bariatric surgery. The major problem they face, however, in accomplishing this is obtaining insurance approval for surgical removal of the excess skin. Most insurance companies consider this "cosmetic" surgery and will not authorize coverage. A few, with appropriate documentation of the conditions and problems from excess skin, do provide coverage for surgery. Plastic surgeons who are experienced in abdominoplasty and body contouring can offer these patients an excellent surgical treatment for the problems of excessive skin. Excess tissue of the lower torso is the most common deformed area for which patients undergo surgical intervention. More radical body contouring can include a circumferential abdominoplasty and lower body lift. Circumferential abdominoplasty removes redundant skin of the lower abdomen, flattens the abdomen, and incorporates the lower body lift. It requires central undermining to the xiphoid and minimal lateral undermining of the superior flap. If simultaneous abdominal hernia repair is performed, this performs the function of fascial imbrication by creating a repair with some degree of fascial tension. The closure of the superior flap to the inferior skin edge incorporates lateral tension to narrow the waist and advance the anterolateral thighs. Medial thighplasty also may be needed for patients with significant excess medial thigh skin. Excess skin redundancy distal to the mid-thighs requires long vertical medial excision of skin. Mid-back and epigastric rolls, along with sagging breasts, are corrected with an upper body lift. The upper body lift is a reverse abdominoplasty, removal of mid-torso excessive skin, and reshaping of the breasts. Increasing numbers of patients undergoing bariatric surgery have provided an increased flow of patients requesting such services, which in turn should lead to improved outcomes with increasing experience for surgeons performing these procedures. One matched control study suggests that plastic surgery after bariatric surgery may actually improve long-term weight loss. Additional problems include skin rashes; maceration under folds in the pannus, thighs, and breasts; body odor; and poorly fitting clothes. Bariatric surgery has been a field of constant succession of procedures in an attempt to improve safety, minimize invasiveness, and offer better outcomes. Recent experimental procedures in electrical stimulation of the stomach and vagus nerves have been performed to produce weight loss. The implantable gastric stimulation device, initially marketed by Trasneuronix, Inc. She desired a one-stage total body lift and bilateral brachioplasties, which were performed in the manner described in the text. A mean excess weight loss of 23% was reported at 16-month follow-up for the second U. The ability to select patients who will respond remains a challenge for this technology, which is still in the status of only a proposed potential operation for weight loss. The scars indicate the circumferential abdominoplasty, lower body lift, upper body lift, breast reshaping, and autoaugmentation through a keyhole pattern and bilateral brachioplasties. All redundant skin has been removed, leaving well-positioned scars and feminine features. Data to date have been sparse and very preliminary in showing any merits of the potential efficacy of this approach. Long-term weight loss of significant magnitude has yet to be demonstrated by these revisional endoscopic procedures. Intragastric balloon placement has resurfaced on the bariatric scene in the past few years. The Garren-Edwards bubble of the late 1980s era196 was prone to migration and bowel obstruction, which led to its early demise. Now this concept has resurfaced as a short-term bridge to weight loss to be followed by a more definitive procedure. While there may be some limited application of this device for such purposes,197 its ability to produce durable weight loss is unproven. It may have potential use only as a preliminary procedure prior to a more definitive one. Prototype procedures undergoing trial include one that uses an endoscopically placed sleeve to limit absorption. A small randomized control study out of the Netherlands compared an endoscopically placed intraluminal sleeve extending from the duodenum to the jejunum (EndoBarrier) to a diet modification control group. Four implants had to be removed before the end of the study due to migration, obstruction, and continuous epigastric pain. The eventual ability to endoscopically create a stapled or sutured gastric pouch and hence a completely endoscopically performed restrictive operation is being envisioned. The human gut micobiome: a review of the effect of obesity and surgically induced weight loss. One-year behavioral treatment of obesity: comparison of moderate and severe caloric restriction and the effects of weight maintenance therapy. Changes in plasma lipids and lipoproteins in overweight men during weight loss through dieting as compared with exercise. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Prevention of type 2 (non-insulindependent) diabetes by diet and physical exercise. Preoperative weight gain does not predict failure of weight loss or co-morbidity resolution of laparoscopic Roux-en-Y gastric bypass for morbid obesity. Effect of preoperative weight loss in bariatric surgical patients: a systematic review. Ten and more years after vertical banded gastroplasty as primary operation for morbid obesity. An experimental evaluation of the nutritional importance of proximal and distal small intestine. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Weight loss and dietary intake after vertical banded gastroplasty and Roux-enY gastric bypass. Laparoscopic adjustable silicone gastric banding in the treatment of morbid obesity. Assessment of predictive ability of Epworth scoring in screening of patients with sleep apnoea. The place of upper gastrointestinal tract endoscopy before and after vertical banded gastroplasty for morbid obesity. Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Risks and benefits of prophylactic inferior vena cava filters in patients undergoing bariatric surgery. Safety and efficacy of simultaneous cholecystectomy at the time of Roux-en-Y gastric bypass. A multicenter, placebo-controlled, randomized, double-blind prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Preoperative weight loss in high-risk superobese bariatric patients: a computed tomography-based analysis. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. A multicenter, prospective, risk-adjusted analysis from the National Surgical Quality Improvement Program. Open versus laparoscopic Roux-en-Y gastric bypass: a comparative study of over 25,000 open cases and the major laparoscopic bariatric reported series. Early results of laparoscopic Swedish adjustable gastric banding for morbid obesity. Laparoscopic adjustable gastric banding: lessons from the first 500 patients in a single institution. Laparoscopic adjustable gastric banding: postoperative management and nutritional evaluation. Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Treatment of morbid obesity and gastroesophageal reflux with hiatal hernia by LapBand. Quality of life after laparoscopic adjustable gastric banding for severe obesity: postoperative and retrospective preoperative evaluations. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 10-year results of a prospective, randomized trial. The effect of Roux limb lengths on outcome after Roux-en-Y gastric bypass: a prospective randomized clinical trial. Small bowel obstruction and internal hernias after laparoscopic Roux-en-Y gastric bypass. Endoscopic intraluminal suture placation of the gastric pouch and stoma in postoperative Roux-en-Y gastric bypass patients. Perioral endoscopic reduction of dilated gastrojejunal anastomosis following Roux-en-Y gastric bypass: a possible new option for patients with weight regain.
Thoracoabdominal aortic aneurysms can cause duodenal obstruction or bacteria 0157 cheap 0.5 mg colchicine otc, if they erode through the bowel wall 600 mg antibiotic order 0.5mg colchicine mastercard, gastrointestinal bleeding oral antibiotics for acne pros and cons discount colchicine 0.5mg with mastercard. Erosion into the inferior vena cava or iliac vein presents with an abdominal bruit zeomic antimicrobial colchicine 0.5mg low cost, widened pulse pressure antibiotic levaquin buy line colchicine, edema antimicrobial wound cream purchase colchicine with amex, and heart failure. Ascending aortic aneurysms can cause displacement of the aortic valve commissures and annular dilatation. The resulting deformation of the aortic valve leads to progressively worsening aortic valve regurgitation. In response to the volume overload, the heart remodels and becomes increasingly dilated. Patients with this condition may present with progressive heart failure, a widened pulse pressure, and a diastolic murmur. Thoracic aortic aneurysms-particularly those involving the descending and thoracoabdominal aorta-are commonly lined with friable, atheromatous plaque and mural thrombus. This debris may embolize distally, causing occlusion and thrombosis of the visceral, renal, or lowerextremity branches. Clinical Manifestations In many patients with thoracic aortic aneurysms, the aneurysm is discovered incidentally when imaging studies are performed for unrelated reasons. However, thoracic aortic aneurysms that initially go undetected eventually create symptoms and signs that correspond with the segment of aorta that is involved. These aneurysms have a wide variety of manifestations, including compression or erosion of adjacent structures, aortic valve regurgitation, distal embolism, and rupture. Patients with ruptured thoracic aortic aneurysms often experience sudden, severe pain in the anterior chest (ascending aorta), upper back or left chest (descending thoracic aorta), or left flank or abdomen (thoracoabdominal aorta). When ascending aortic aneurysms rupture, they usually bleed into the pericardial space, producing acute cardiac tamponade and death. Descending thoracic aortic aneurysms rupture into the pleural cavity, producing a combination of severe hemorrhagic shock and respiratory compromise. External rupture is extremely rare; saccular syphilitic aneurysms have been observed to rupture externally after eroding through the sternum. Diagnostic Evaluation Diagnosis and characterization of thoracic aneurysms require imaging studies, which also provide critical information that 790 guides the selection of treatment options. Although the best choice of imaging technique for the thoracic and thoracoabdominal aorta is somewhat institution-specific, varying with the availability of imaging equipment and expertise, efforts have been made to standardize key elements of image acquisition and reporting. Recent practice guidelines40 recommend that aortic imaging reports plainly state the location of aortic abnormalities (including calcification and the extent to which abnormalities extend into branch vessels), the maximum external aortic diameters (rather than internal, lumen-based diameters), internal filling defects, and any evidence of rupture. Whenever possible, all results should be compared to those of prior imaging studies. Plain radiographs of the chest, abdomen, or spine often provide enough information to support the initial diagnosis of thoracic aortic aneurysm. Ascending aortic aneurysms produce a convex shadow to the right of the cardiac silhouette. The anterior projection of an ascending aneurysm results in the loss of the retrosternal space in the lateral view. Aortic root aneurysms, for example, often are hidden within the cardiac silhouette. Once a thoracic aortic aneurysm is detected on plain radiographs, additional studies are required to define the extent of aortic involvement. Ascending aortic aneurysms are commonly discovered during echocardiography in patients presenting with symptoms or signs of aortic valve regurgitation. Both transthoracic and transesophageal echocardiography provide excellent visualization of the ascending aorta, including the aortic root. Effective echocardiography requires considerable technical skill, both in obtaining adequate images and in interpreting them. This imaging modality has the added benefit of assessing cardiac function and revealing any other abnormalities that may be present. During ultrasound evaluation of a suspected infrarenal abdominal aortic aneurysm, if a definitive neck cannot be identified at the level of the renal arteries, the possibility of thoracoabdominal aortic involvement should be suspected and investigated by using other imaging modalities. Caution should be exercised while interpreting aneurysm dimensions from ultrasound imaging because intraluminal measurements are often reported, whereas external measurements are usually used in other imaging modalities. Chest radiographs showing a calcified rim (arrows) in the aortic wall of a thoracoabdominal aortic aneurysm. If renal insufficiency occurs or is worsened, elective surgery is postponed until renal function returns to normal or stabilizes. Although catheter-based contrast aortography was previously considered the gold standard for evaluating thoracic aortic disease, cross-sectional imaging. Today, the use of invasive aortography in patients with thoracic aortic disease is generally limited to those undergoing endovascular therapies or when other types of studies are contraindicated or have not provided satisfactory results. Unlike standard aortography, cardiac catheterization continues to play an important role in diagnosis and preoperative planning, especially in patients with ascending aortic involvement. Proximal aortography can reveal not only the status of the coronary arteries and left ventricular function but also the degree of aortic valve regurgitation, the extent of aortic root involvement, coronary ostial displacement, and the relationship of the aneurysm to the arch vessels. The value of the information one can obtain from catheterbased diagnostic studies should be weighed against the established limitations and potential complications of such studies. A key limitation of aortography is that it images only the lumen and may therefore underrepresent the size of large aneurysms that contain laminated thrombus. Manipulation of intraluminal catheters can result in embolization of laminated thrombus or atheromatous debris. Other risks include allergic reaction to contrast agent, iatrogenic aortic dissection, and bleeding at the arterial access site. In addition, the volumes of contrast agent required to adequately fill large aneurysms can cause significant renal toxicity. Current practice guidelines40 seek to standardize the reporting of aortic diameters by indicating key locations of measurement. These include (1) the sinuses of Valsalva, (2) the sinotubular junction, (3) the mid-ascending aorta, (4) the proximal aortic arch at the origins of the innominate artery, (5) the mid-aortic arch, which is between the left common carotid and left subclavian arteries, (6) the proximal descending thoracic aorta, which begins at the isthmus (approximately 2 cm distal to the origins of the left subclavian artery), (7) the mid-descending thoracic artery, (8) the aorta at the diaphragm, and (9) the abdominal aorta at the origins of the celiac axis. Once a thoracic aortic aneurysm is detected, management begins with patient 792 education, particularly if the patient is asymptomatic, because aortic disease may progress rapidly and unexpectedly in some patients. A detailed medical history is collected, a physical examination is performed, and a systematic review of medical records is carried out to clearly assess the presence or absence of pertinent symptoms and signs, despite any initial denial of symptoms by the patient. Signs of genetic diseases such as Marfan syndrome or Loeys-Dietz syndrome are thoroughly reviewed. If clinical criteria are met for such a genetic condition, confirmatory laboratory tests are conducted. Patients with such genetic diseases are best treated in a dedicated aortic clinic where they can be appropriately followed up. Surveillance imaging and aggressive blood pressure control are the mainstays of initial management for asymptomatic patients. When patients become symptomatic or their aneurysms grow to meet certain size criteria, the patients become surgical candidates. Although long-term data are still lacking, endovascular therapy has become an accepted treatment for thoracic aortic aneurysms. Food and Drug Administration for the treatment of isolated descending thoracic aortic aneurysms, and some newer devices are approved for the treatment of blunt aortic injury and penetrating aortic ulcer. In practice, however, the off-label application 3 of aortic stent grafts is widespread and accounts for well over half their use. Despite these advances, for the repair of aneurysms with proximal aortic involvement and of thoracoabdominal aortic aneurysms, open procedures remain the gold standard and preferred approach. Crosssectional imaging with reconstruction is critical when one is evaluating a thoracic aneurysm, determining treatment strategy, and planning necessary procedures. Note that, commonly, patients with a thoracic aortic aneurysm also have a remote aneurysm. In many patients, staged operative procedures are necessary for complete repair of extensive aneurysms involving the ascending aorta, transverse arch, and descending thoracic or thoracoabdominal aorta. An important benefit of this approach is that it allows treatment of valvular and coronary artery occlusive disease at the first operation. Proximal aneurysms (proximal to the left subclavian artery) usually are addressed via a sternotomy approach. Aneurysms involving the descending thoracic aorta are evaluated in terms of criteria (described later) for potential endovascular repair; those unsuitable for an endovascular approach are repaired with open techniques through a left thoracotomy. These details are important in preventing embolization during surgical manipulation. Indications for Operation Thoracic aortic aneurysms are repaired to prevent fatal rupture. Therefore, on the basis of the natural history studies and other data, practice guidelines for thoracic aortic disease40 recommend elective operation in 4 asymptomatic patients when the diameter of an ascending aortic aneurysm is >5. In patients with connective tissue disorders such as Marfan and Loeys-Dietz syndromes, the threshold for operation is based on a smaller aortic diameter (4. For women with connective tissue disorders who are considering pregnancy, prophylactic aortic root replacement is considered because the risk of aortic dissection or rupture increases at an aortic diameter of 4. For lowrisk patients with chronic aortic dissection, descending thoracic repair is recommended at an aortic diameter of 5. For patients undergoing aortic valve replacement or repair, 5 smaller ascending aortic aneurysms (>4. The acuity of presentation is a major factor in decisions about the timing of surgical intervention. Many patients are asymptomatic at the time of presentation, so there is time for thorough preoperative evaluation and improvement of their current health status, such as through smoking cessation and other optimization programs. Symptomatic patients are at increased risk of rupture and warrant expeditious evaluation. The onset of new pain in patients with known aneurysms is especially concerning, because it may herald significant expansion, leakage, or impending rupture. Emergent intervention is reserved for patients who present with aneurysm rupture or superimposed acute dissection. Endovascular Repair As noted earlier, endovascular repair of thoracic aortic aneurysms has become an accepted treatment option in selected patients, particularly patients with isolated degenerative descending thoracic aortic aneurysms; in fact, practice guidelines recommend that endovascular repair be strongly considered for patients with descending thoracic aneurysm at an aortic diameter of 5. For one, the proximal and distal neck diameters should fall within a range that will allow proper sealing. Also, the proximal and distal landing zones should ideally be at least 20 mm long so that an appropriate seal can be made. Note that the limiting structures proximally and distally are the brachiocephalic vessels and celiac axis, respectively. Another anatomic limitation for this therapy relates to vascular access: the femoral and iliac arteries have to be wide enough to accommodate the large sheaths necessary to deploy the stent grafts, although newer devices use a smaller sheath (or are "sheathless" self-deployed stent grafts) to accommodate smaller arteries. Tortuosity of the iliac vessels and abdominal aorta can make these procedures technically challenging. Occasionally, a "side graft" anastomosed to the iliac artery through a retroperitoneal incision is used because of poor distal access. When any of these anatomic criteria are not met, an open approach is preferable to an endovascular approach. Of note, attempts have been made to extend the use of endovascular therapy to aortic arch aneurysms and thoracoabdominal aortic aneurysms. Additionally, there have been numerous reports of small series of offlabel, experimental hybrid procedures that involve debranching the aortic arch or the visceral vessels of the abdominal aorta, followed by endovascular exclusion of the aneurysm. In its simplest form, hybrid arch repair involves an open bypass from the left subclavian to the left common carotid artery, which is followed by deliberate coverage of the origins of the left subclavian artery by the stent graft. In its most complex form, hybrid arch repair involves rerouting all of the brachiocephalic vessels, followed by proximal placement of the stent graft in the ascending aorta and extending repair distally into the aortic arch and descending thoracic aorta. The patients who theoretically may benefit more from an endovascular approach than from traditional open techniques are those who are of advanced age or have significant comorbidities. For example, the open repair of a descending thoracic aortic aneurysm can result in significant pulmonary morbidity. Therefore, patients with borderline pulmonary reserve may better tolerate an endovascular procedure than standard open repair. In contrast, patients with significant intraluminal atheroma may be better served by an open approach because of the risk of embolization and stroke posed by catheter manipulation. Similarly, patients with connective tissue disorders generally are not considered candidates for elective endovascular repair. Endovascular repair in patients with connective tissue disorders has produced poor results, which are mainly due to progressive dilatation, stent graft migration, and endoleak. In suitable patients, borderline pulmonary function can be improved by implementing a regimen that includes smoking cessation, weight loss, exercise, and treatment of bronchitis for a period of 1 to 3 months before surgery. In such patients, preserving the left recurrent laryngeal nerve, the phrenic nerves, and diaphragmatic function is particularly important. Renal Evaluation Renal function is assessed preoperatively by measuring serum electrolyte, blood urea nitrogen, and creatinine levels. Information about kidney size and perfusion can be obtained from the imaging studies used to evaluate the aorta. Obtaining accurate information about baseline renal function has important therapeutic and prognostic implications. For example, perfusion strategies and perioperative medications are adjusted according to renal function. Patients with severely impaired renal function frequently require at least temporary hemodialysis after surgery. These patients also have a mortality rate that is significantly higher than normal. Patients with thoracoabdominal aortic aneurysms and poor renal function secondary to severe proximal renal occlusive disease undergo renal artery endarterectomy, stenting, or bypass grafting during the aortic repair.


















